New psychoactive substances: health and social responses
Introduction
This miniguide is one of a larger set, which together comprise Health and social responses to drug problems: a European guide. It provides an overview of the most important aspects to consider when planning or delivering health and social responses to problems related to new psychoactive substances, and reviews the availability and effectiveness of the responses. It also considers implications for policy and practice.
Last update: 26 October 2021.
Contents:
Overview
Key issues
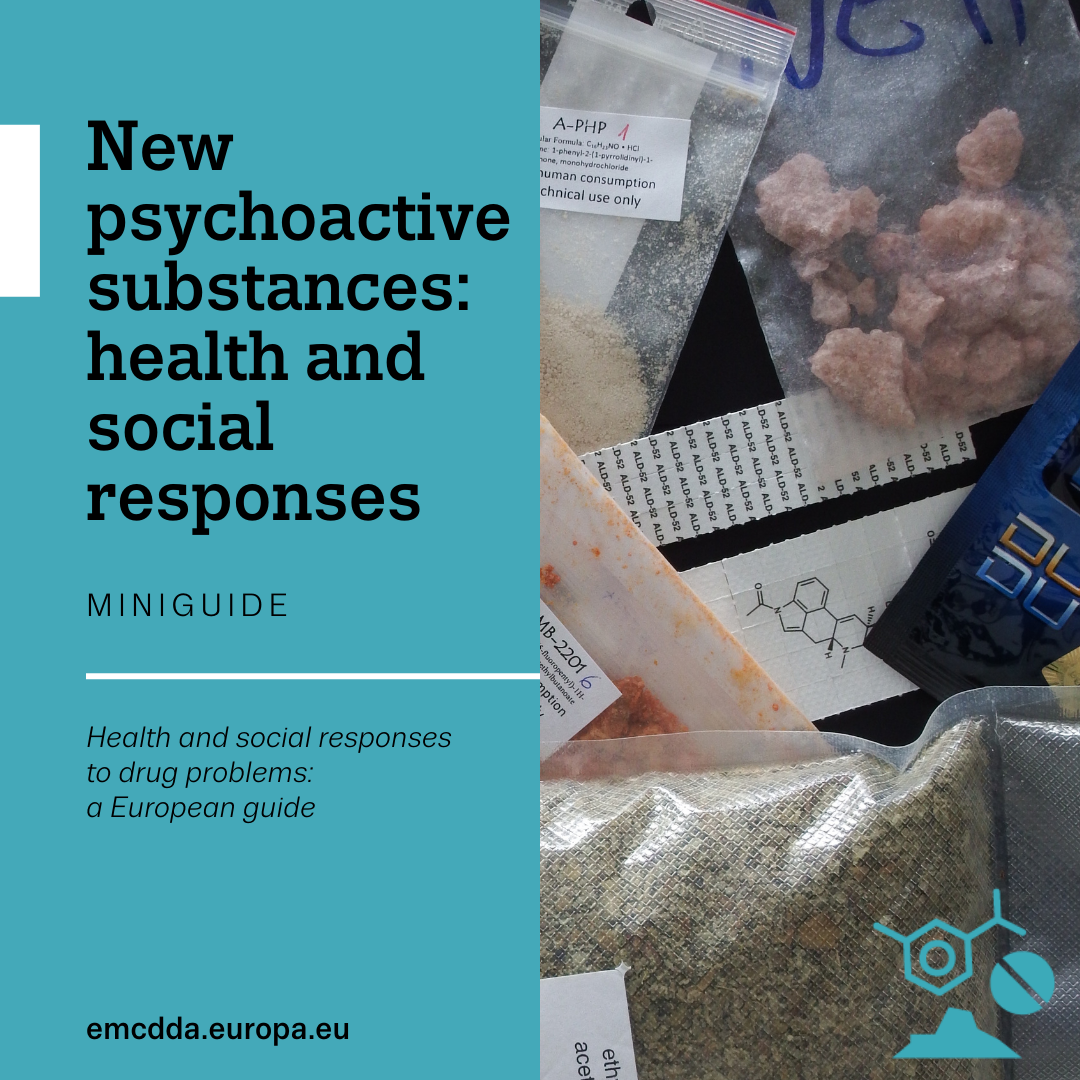
The term new psychoactive substances is used for a broad range of chemicals or compounds that are consumed, or made available for human consumption, for their psychoactive properties but that are not controlled under the United Nations drug control conventions. For the purposes of this miniguide, the term covers a wide range of new and novel substances that present in many respects similar challenges when it comes to developing health and social interventions.
New psychoactive substances may pose health and social threats that are similar to those associated with better-known controlled substances and often appear in the same broad chemical classes (opioids, benzodiazepines, stimulants, etc.). Yet they are chemically different, so the risks they present to health may differ or simply be unknown.
New psychoactive substances may be purchased from online retailers, social media, or sometimes from high-street suppliers and marketed as ‘legal’ replacements for illicit drugs. They may also be sold together with, or as, other better-known controlled substances, meaning that those using them may be unaware of what they are consuming.
New psychoactive substances are used by different groups, including people who take drugs recreationally. Due to the relatively low cost and high potency of some new psychoactive substances, they are also increasingly being used by marginalised groups, for example the homeless or people with long-term and highly problematic drug use. In addition, because new psychoactive substances are harder to detect and identify in routine urine testing, they may be used by people who are regularly subjected to drug testing procedures and wish to avoid their drug use being detected. Moreover, the fact that such high-potency substances may be relatively easy to conceal means that, in some countries, their use within the prison population is regarded as problematic.
The large number of substances that can be categorised as new psychoactive substances, their chemical diversity and the speed with which they appear are all challenging factors in both monitoring the problem and developing effective and timely responses.
Evidence and responses
Possible interventions include:
- Early warning and risk assessment systems supported by data from forensic and toxicology laboratory networks on the chemical identification of new psychoactive substances.
- Consumer safety and other regulatory approaches that are intended to limit the availability of new psychoactive substances and restrict open sales.
- Risk communication with health authorities, professionals and people who use drugs related to harmful new substances.
- The inclusion of components on new substances in both prevention and harm reduction programmes, with specific education and harm reduction messages targeted at those already using drugs or at risk of taking new substances.
- Making training and awareness-raising activities available for professionals in prevention, treatment and harm reduction services in order to enhance their competencies in identifying and responding to the use of new substances.
- Developing clinical guidelines for the management of acute toxicity caused by new psychoactive substances.
- Drug-checking services that may also potentially support early warning systems and provide a conduit for delivering information, advice and brief interventions to people who use new psychoactive substances.
- Multidisciplinary approaches: the linking of different services may be needed to engage vulnerable groups who otherwise might not come into contact with traditional services.
In general, health and social responses to new substances are often adaptations of programmes created to deal with more established drugs.
European picture
- EU legislation provides a three-step approach – comprising early warning, risk assessment and control measures – that allows countries to rapidly detect, assess and respond to public health and social threats caused by new psychoactive substances. The EMCDDA plays a central role in this system.
- Multidisciplinary harm reduction approaches are being developed and trialled in which vulnerable groups who may not otherwise come into contact with drug services are being engaged, for example through sexual health settings or services working with the homeless.
- Clinical guidelines for the treatment of acute intoxications associated with new psychoactive substances are being developed and published. In some countries, specific guidance on responding to the use of these substances in prisons and custodial settings is also under development.
- Harm reduction information platforms, often coupled with drug checking, are operating in a number of countries and online.
- Specialist treatment for problems caused by new substances is not well developed in most countries.
Key issues: patterns of new psychoactive substance use and related harms
The key questions that need to be addressed when identifying and defining a problem include who is affected, what types of substances and patterns of use are involved, and where is the problem occurring? Responses should be tailored to the particular drug problems being experienced, and these may differ between countries and over time. The wide array of factors that have to be considered at this stage in the process are discussed in the Action framework for developing and implementing health and social responses to drug problems.
In Europe, the term new psychoactive substances is legally defined for the purposes of the EU early warning and risk assessment system as a substance, in pure form or in a preparation, that is not covered by the 1961 United Nations Single Convention on Narcotic Drugs, as amended by the 1972 Protocol, or by the 1971 United Nations Convention on Psychotropic Substances but may pose health or social risks similar to those posed by the substances covered by those conventions (Article 1 of Council Framework Decision 2004/757/JHA as amended).
More generally, the term new psychoactive substances is often used less specifically and in a non-technical manner to refer to a broad range of chemicals or compounds that are consumed, or made available for human consumption, for their psychoactive properties but that are not necessarily controlled under the United Nations drug control conventions. The reader should therefore be aware that the definition of what is considered a new psychoactive substance may vary according to context and in time. For example, some substances that were historically identified as new psychoactive substances, such as mephedrone, have subsequently been controlled internationally but may still sometimes be referred to as a new psychoactive substance in some contexts. For the purposes of this mini-guide, the term is used quite broadly to cover a wide range of new and novel substances that present in many respects similar challenges when it comes to developing health and social interventions.
New psychoactive substances may pose health and social threats that are similar to those associated with controlled substances. They also often appear in the same broad chemical classes as better-known controlled substances, with many new psychoactive substances being classified as synthetic cannabinoids, opioids, benzodiazepines, stimulants and hallucinogens. However, as they are chemically different to established drugs, the risks they pose to health may differ and, for many new substances, simply be unknown.
New psychoactive substances may be purchased from online retailers and social media platforms or sometimes from high street suppliers, and in some cases they may be marketed as ‘legal’ replacements for illicit drugs. However, a number of countries have introduced regulations to limit their availability and open sale. This means that in some countries their sale on the open market has become less common, while at the same time their availability on the illicit drug market has grown. New psychoactive substances are also sold alongside controlled substances on illicit drug markets, often in combination with, or as, other better-known controlled substances, meaning that those using them may be unaware of what they are consuming.
Since around 2008, there has been a great increase in the availability of new psychoactive substances in Europe. As the range of new substances and products has grown, so have the groups of people who use them. Initially, most people who used new psychoactive substances were those seeking novel experiences and effects (often called ‘psychonauts’), as well as groups such as electronic dance music fans and clubbers.
The relatively low cost and high potency of some new psychoactive substances compared with more established controlled substances have also meant that problems related to new psychoactive substances appear to be increasing in marginalised and excluded communities. Those who use these substances now include a broader range of people, such as recreational drug users, people who self-medicate, individuals looking to improve their appearance or performance, vulnerable groups, for instance people experiencing homelessness, and people engaged in high-risk drug use (including those who inject opioids). Because new psychoactive substances are harder to detect and identify in routine testing, people who use them also include those who are regularly subjected to drug testing procedures, such as people in prison, people in drug treatment, drivers, and those subjected to workplace drug testing.
Concerns have also been raised in a number of European countries about the use of new psychoactive substances and established illicit drugs, including mephedrone, GHB/GBL and methamphetamine, by men who have sex with men and take such substances to enhance, sustain, disinhibit or facilitate sexual pleasure. This practice, sometimes referred to as ‘chemsex’, is associated with high-risk drug use and sexual behaviour (e.g. injecting, unprotected sex, sex with multiple partners), potentially resulting in hospitalisation, overdose, sexually transmitted infections, and infection with HIV and HCV (Spotlight on… Addressing sexual health issues associated with drug use).
New psychoactive substances have been linked to a range of harms. These include non-fatal and fatal poisonings and the spread of drug-related infectious diseases and bacterial infections. In some cases, such outcomes have been noted in the form of outbreaks which place substantial demands on healthcare systems. Currently, synthetic opioids, such as fentanyl derivatives and synthetic cannabinoids, pose particular challenges to public health.
Synthetic opioids are sometimes sold as, or mixed with, heroin or other illicit drugs. They are also used to make fake medicines. The risk of severe and fatal poisoning may thus be increased, both among people engaged in high-risk opioid use and other groups who have not built up a tolerance to opioids. The high potency of these substances may also pose a serious risk to the family and friends of those who use new psychoactive substances, through accidental exposure, as well as to first responders, forensic personnel, postal service workers and staff in custodial settings (see Spotlight on… Fentanils and other new opioids).
Over the last few years, there appears to have been an increase in the number and availability of new benzodiazepines, such as etizolam and flualprazolam. Of particular concern is the growing use of new benzodiazepines to create fake tablets of commonly prescribed benzodiazepine medicines, such as diazepam (Valium) and alprazolam (Xanax), which are often sold at very low prices. The use of these substances in combination with opioids or alcohol may increase the risk of overdose or other negative consequences, such as violent or self-harming behaviour.
Synthetic cannabinoids are often highly potent substances that were initially sold as ‘legal alternatives’ to cannabis. In recent years, it has become more common for certain groups to seek out these substances for their effects. In prisons, the use and distribution of synthetic cannabinoids has been associated with issues such as debt and bullying, as well as aggression and violence (see Spotlight on… Synthetic cannabinoids). Harms associated with synthetic cannabinoids may be more severe than, or altogether different from, those associated with plant-based cannabinoids, and may result in fatalities. In addition, recent evidence suggests that, compared with cannabis, synthetic cannabinoids are more likely to lead to dependence and may entail more serious withdrawal symptoms. Recently, cannabis products adulterated with synthetic cannabinoids have been reported in a number of countries, and linked to both non-fatal intoxications and, in some cases, deaths. This is a particularly worrying development given the relatively large number of cannabis consumers in comparison to users of other drugs and the high potency and known toxicity of some of the synthetic cannabinoids that have been detected in recent years.
Synthetic cathinones have effects similar to known stimulant drugs and are structurally related to cathinone, which is found in the khat plant (Catha edulis). The use of synthetic cathinones as stimulants has been observed in some groups. These substances may sometimes be sold as, or mixed with, other stimulants, such as cocaine, amphetamines or MDMA. Mephedrone was one of the first synthetic cathinones to come to the notice of the public, attracting considerable attention as a so-called ‘legal high’ that appeared on the market in many countries before European-level control measures were introduced in 2010. The psychological side-effects of synthetic cathinones can include an unpleasant ‘comedown’, depression, anxiety, panic attacks, paranoia and psychosis. Compulsive use and dependence symptoms have also been reported by people who use synthetic cathinones. The use of synthetic cathinones has also been noted in some groups of people who inject drugs and has been associated with a risk of tissue damage and severe bacterial or viral infections. Indeed, the injecting of synthetic cathinones has been linked to documented outbreaks of HIV in some countries.
Problems associated with the use of new psychoactive substances are often seen in presentations to emergency departments associated with drug toxicity. The Euro-DEN Plus network of sentinel hospitals in 21 European countries found that new psychoactive substances were typically implicated in around one in 10 presentations. Significant geographical and temporal variations were observed in the involvement of new psychoactive substances in hospital presentations, in one reporting period ranging from none at all to more than one in five, depending on the emergency department concerned.
Assessment of the prevalence and consequences of the use of new psychoactive substances is also complicated, because new and novel substances may be difficult to identify without the support of specialist forensic or toxicological services, and the introduction of new substances may be missed by established routine screening procedures. The situation is further complicated by the fact that those who use new psychoactive substances are often misinformed or unaware of what substances they have consumed. This means self-reported data may be unreliable in identifying the actual substances that have been taken. Additional challenges to monitoring and responding are posed by the ways in which new psychoactive substances may be sold – in the form of mixtures, or as branded products whose constituent elements change over time, or instead of controlled drugs or mixed with them. As a result of these challenges, our understanding of patterns of new psychoactive substance use remains poor, with most information coming from case studies of populations and settings where problems have occurred. Nonetheless, the information available is sufficient to identify a range of settings in which interventions targeting problems associated with new psychoactive substances are likely to be appropriate.
The difficulty in accurately identifying what substances are being consumed and a lack of understanding of the potential risks associated with the consumption of novel substances also can present problems in terms of engaging with potential consumers and encouraging the adoption of appropriate harm reduction and help-seeking behaviours, especially where people are unaware of what substance they have taken. Consumers may also erroneously believe that if a substance appears to be ‘legally’ available, the risks of consumption will be lower than those associated with better-known controlled substances. This problem may be exacerbated if new psychoactive substances are marketed as wellness or study aids or alternatives to medicinal products.
Evidence and responses to new psychoactive substance-related problems
Choosing appropriate responses that are likely to be effective in dealing with a particular drug-related problem requires a clear understanding of the primary objectives for the intervention or combination of interventions. Ideally, interventions should be supported by the strongest available evidence; however, when evidence is very limited or unavailable, expert consensus may be the best option until more conclusive data can be obtained. The Action framework for developing and implementing health and social responses to drug problems discusses in more detail what to bear in mind when selecting the most appropriate response options.
A number of challenges exist with respect to monitoring and developing effective and timely responses, namely the large number of new psychoactive substances that can potentially be used, their chemical diversity and the speed at which they appear on the market. In addition, there is often a lack of capacity to detect and report on acute harms (and link these to a particular substance), as well as limited information on the pharmacology and toxicology of these substances.
Alongside early warning systems and regulatory controls, other responses include specialised treatment, educational responses (e.g. the dissemination of educational material), harm reduction measures (e.g. the provision of sterile injecting equipment) and the medical treatment of overdoses (e.g. symptomatic management of acute emergencies and the administration of antidotes).
Responses to new substances often involve adapting evidence-based responses to reducing the harms associated with established drugs. Adjustments may need to take account of specific drug effects, the socio-cultural characteristics of certain risk groups (e.g. partygoers or men who have sex with men) or particular risk behaviours (e.g. increased access to syringes in response to high injecting frequency or the proposal of alternative routes of administration).
Monitoring and early warning
It is essential to know which new psychoactive substances are being sold and used in order to develop appropriate responses. Early warning systems and related monitoring systems play a central role in identifying and responding rapidly to emerging harms caused by new substances. These systems need to be based on data regarding the chemical identification of new substances from forensic and toxicology laboratory networks related to law enforcement seizures and cases of poisoning, and draw on information from a wide range of sources, potentially including law enforcement, treatment and low-threshold services, poison centres, hospital emergency departments and medico-legal death investigations.
Drug-checking services may also potentially support early warning systems and provide a conduit for the provision of information, advice and brief interventions to people who use new psychoactive substances. More novel data sources, such as the analysis of wastewater and other urine samples, as well as analysis of drug residues from used syringes and drugs collected from amnesty bins, may also have potential to support surveillance in this area.
Prevention
Prevention interventions which stress skills and coping strategies are effective, independently of the substance. When new psychoactive substances are included in school-based prevention activities, it would be most appropriate to do this as part of a generic prevention programme that is supported by evidence of effectiveness. Components incorporating the discussion of new substances might focus on providing accurate descriptive and injunctive norms. For example, based on local data, this may include messages such as, ‘very few people use new substances’ and ‘young people like you say they don’t want to take risks with unknown substances’. More specific education and harm reduction interventions targeting new substances are likely to be most appropriate for individuals who are either already using drugs or at increased risk of doing so, or in settings where the risks of new psychoactive substance use are known to be elevated.
Clinical settings
Clinical practice in the treatment of new psychoactive substance-related problems, including dependence, withdrawal and acute toxicity, is broadly comparable to that for the corresponding groups of established substances. This is so because the harms experienced are similar (with the exception of synthetic cannabinoids, see Spotlight on… Synthetic cannabinoids), while in cases of acute toxicity there is generally limited capacity to check, in a timely manner, for the presence of new psychoactive substances. With regard to synthetic opioids, due to their higher potency, overdose treatment is likely to call for further action, such as higher doses of naloxone and longer periods of observation in a clinical setting (see Spotlight on… Fentanils and other new opioids). This is in line with clinical guidelines developed elsewhere for responding to acute and chronic health harms related to new psychoactive substances, such as, for example, the Novel Psychoactive Treatment UK Network (Neptune).
As healthcare professionals may feel unskilled when first confronted by problems caused by new substances, basic knowledge-sharing, competence-building and highlighting how to transfer existing competencies to new substances are also important. For instance, the Drugs Wheel is a model that can be used a resource and training tool for health and clinical staff. Available online in several European languages, it classifies drugs, including new psychoactive substances, within a number of categories (e.g. opioids, stimulants, psychedelics), allowing clinical staff to provide treatment, advice and harm reduction information without detailed knowledge of every compound.
Non-fatal and fatal poisonings associated with new psychoactive substances have been observed. These sometimes manifest as outbreaks of multiple cases appearing over a relatively short period and within a restricted geographical area. Such outbreaks have highlighted the need to establish information exchange systems to coordinate a rapid response in similar situations and effectively communicate risks. It is important to provide appropriate information on new psychoactive substances to people who use drugs, practitioners and policymakers, but also to the public at large in order to avoid sensationalist media reports and pre-empt possible public fears. A risk communication strategy can form a useful component of response planning in this area. Attention should be focused on what sort of information is communicated, who receives it and what implications this may have for further action. Consideration should also be given to identifying and reducing any possible unintended negative consequences of miscommunication. For example, media accounts that place emphasis on particular substances as being especially powerful or strong may encourage consumer interest rather than diminish it.
Cultural competence
Cultural competence (an understanding of how cultural issues influence patterns of drug use and associated harms) is required to ensure service engagement and uptake. This means that services need to be accessible and welcoming to all groups of potential clients. Staff in services seeking to attract those who are experiencing problems with new psychoactive substances may need to undergo training to develop the competencies necessary to work with diverse groups of people who use new substances, many of whom will not have previously presented to drug services primarily focused on established illicit drugs. Appropriate cultural competence may be a particularly important consideration for the design of interventions in this area that are targeting specific subpopulations or settings.
Harm reduction
A particular challenge lies in delivering interventions to hard-to-reach populations of people who use new psychoactive substances and who are experiencing, or are at elevated risk of experiencing, significant harms. Research in this area has identified a number of groups that may fall into this category, for example people with long-term chronic drug problems (including those who inject drugs), men who have sex with men and who practise ‘chemsex’, psychonauts homeless people and people in prison. Multidisciplinary responses and collaborations between health and other service providers in various settings (e.g. sexual health clinics, custodial settings and drug treatment centres) are therefore likely to be needed to reduce harms in these populations (see, for example, Spotlight on… Addressing sexual health issues associated with drug use).
The internet is increasingly used to provide information and counselling, including ‘online-outreach’ interventions to reach new target groups. Examples in this area include user-led initiatives by people who use new psychoactive substances, such as forums and blogs, which provide consumer protection information, advice and so-called ‘trip records’ that describe the experiences of people who have already used a particular new substance (giving details such as the setting where it was taken, quantity, time of onset, effects and ‘coming-down’ phase). The impact and accuracy of these services is not known and they could potentially provide misleading information as well as valuable advice. In a few cases, these interventions have been linked with drug-checking services, with results and harm reduction messages disseminated online and via mobile apps. Currently, there remains a need for more research in the area of risk communication and the evaluation of different models in providing information on new psychoactive substances to people who use them.
European picture: availability of new psychoactive substance-related interventions
Early warning systems and regulatory approaches
A three-step legal framework of early warning, risk-assessment and control measures allows the European Union to rapidly detect, assess and react to public health and social threats caused by new psychoactive substances. The EMCDDA is responsible for the first two steps in this system, namely operating an early warning system with the cooperation of Europol (the EU police agency) and conducting risk assessments. The European Commission is responsible for proposing control measures.
Alongside developing early warning systems, initial responses to the emergence of new psychoactive substances in Europe have been predominantly regulatory in nature, using legislative tools to reduce their supply. Actions have also been taken in producer countries, for example restrictions have recently been imposed in response to the growing global awareness of the health impacts of fentanyl derivatives. The challenge for legislative responses posed by the adaptability of the new psychoactive substance market is illustrated by the fact that (possibly in response to regulatory changes) of the 10 new synthetic opioids detected for the first time in Europe in 2020 by the EU Early Warning System, nine did not belong to the fentanyl group, although they still potentially presented a similar threat to public health.
Treatment
Specialist treatment for new psychoactive substance-related harms is not well developed in most European countries. There is also a limited demand in Europe for specialist drug treatment for problems caused by the use of new substances. This may be related to a number of factors, for example poor identification of use, low prevalence of use and low levels of problematic use; or it may be that many of the substances appearing in this category are more associated with acute rather than chronic problems such as dependence. Poor identification of use may reflect an under-reporting of use or the misreporting of substances (as people who use these drugs might not know what they are taking), a lack of suitable screening and monitoring instruments and low professional awareness of new substances.
Nevertheless, service developments are now being seen in a number of countries. Clinical guidelines for responding to acute and chronic health harms are being developed in some European countries, and more attention is being paid to developing targeted education and prevention activities and to instigating training and awareness-raising activities for professionals. Specific guidance on responding to the use of new psychoactive substances in prisons and other custodial settings is also being developed in some countries.
Harm reduction
Health and social responses to the challenges posed by new drugs have been slow to emerge, but are now gathering momentum in Europe. These include a wide range of initiatives mirroring the full spectrum of responses to established illicit substances, such as drug education and training activities, user-led consumer protection interventions on the internet, and needle and syringe programmes in low-threshold services.
The emergence of new substances has manifested itself in various forms in different countries, and national responses reflect these differences. In Hungary and Romania, where injecting synthetic cathinones has been reported, needle and syringe exchange services play an important role. In the United Kingdom, where significant use of mephedrone has been noted, specialist ‘club-drug clinics’ have been developed to engage with this client group.
Services working in nightlife and recreational settings have tended to integrate their responses to new psychoactive substances within established approaches. Some NGOs and online platforms, such as TechnoPlus and PsychoActif, provide detailed instructions on how to test new psychoactive substances for allergic and adverse reactions before use. One innovative harm reduction programme, HaRePo, was established in France by the NGO SAFE. HaRePo provides harm reduction counselling by phone and email, and sends harm reduction tools through the French postal service. The programme is free and confidential and has been successful in reaching people who use drugs and are not familiar with low-threshold services, including a high number of men who have sex with men and who practise chemsex using cathinones.
Implications for policy and practice
Basics
Core interventions in this area include:
- Early warning systems to monitor new substances on the market and the harms they cause. These need to be supported by the chemical identification of new substances by forensic and toxicology laboratory networks.
- The provision of training materials on new substances for health professionals and the creation of knowledge exchange platforms for clinicians, healthcare professionals and social workers at the local and national level.
- Interventions addressing the use of new psychoactive substances based on responses to established drug groups, but adapted appropriately to account for the nature and patterns of use of these new substances, different user groups and the specific contexts in which use takes place.
Opportunities
- Where appropriate, national health authorities should be encouraged to develop new psychoactive substance guidelines, including guidance on overdose management. Alternatively, guidelines developed elsewhere, such as the UK-based NEPTUNE Guidance, may be translated and adapted to meet national needs.
- Analytical and toxicological testing and risk-assessment capacities need to be enhanced and results disseminated in a timely and usable way to both risk groups and relevant professionals.
- Services need to be developed to address the specific issues of use associated with new psychoactive substances among particular groups, such as the homeless, people in prison and people who inject drugs.
Gaps
- The effectiveness of the adapted interventions currently being used for responding to new substances should be evaluated.
- The impact of different ways of communicating the risks associated with new psychoactive substances is not well understood. Therefore, there is a need to develop and strengthen the evidence base in the area of risk communication.
- To improve the targeting and development of appropriate responses, in addition to fundamental research (in pharmacology and toxicology), better epidemiological data is required on the extent of the use of new psychoactive substances and the motivations for use as well as patterns of use and how they change over time.
Further resources
EMCDDA
- Best practice portal.
- EMCDDA resources on new psychoactive substances (NPS).
- EU Early Warning System on new psychoactive substances.
- Synthetic cannabinoids in Europe – a review, 2021.
- New benzodiazepines in Europe – a review, 2021.
- European drug report 2021: trends and developments
- New psychoactive substances: global markets, glocal threats and the COVID-19 pandemic, 2020.
- Fentanils and synthetic cannabinoids: driving greater complexity into the drug situation. An update from the EU Early Warning System, 2018.
- Drug checking as a harm reduction tool for recreational drug users: opportunities and challenges, 2017.
- New psychoactive substances in Europe: legislation and prosecution — current challenges and solutions, 2016.
- Injection of synthetic cathinones, Perspectives on drugs, 2015.
- New psychoactive substances in Europe: Innovative legal responses, 2015.
Other sources
- UNODC, Global SMART programme.
- Novel Psychoactive Substances. Classification, pharmacology and toxicology, 2nd edition, 2021.
- Amy Peacock, PhD Raimondo Bruno, PhD Natasa Gisev, PhD Prof Louisa Degenhardt, PhD Prof Wayne Hall, PhD Roumen Sedefov, MD et al., New psychoactive substances: challenges for drug surveillance, control, and public health responses, The Lancet, 2019.
- Neptune group, Neptune clinical guidance, 2015.
About this miniguide
This miniguide provides an overview of what to consider when planning or delivering health and social responses to stimulant-related problems, and reviews the available interventions and their effectiveness. It also considers implications for policy and practice. This miniguide is one of a larger set, which together comprise Health and Social Responses to Drug Problems: A European guide.
Recommended citation: European Monitoring Centre for Drugs and Drug Addiction (2021), New psychoactive substances: health and social responses, https://www.emcdda.europa.eu/publications/mini-guides/new-psychoactive-….
Identifiers
HTML: TD-03-21-333-EN-Q
ISBN: 978-92-9497-670-3
DOI: 10.2810/243938