Perspectives on drugs: strategies to prevent diversion of opioid substitution treatment medications
Introduction
Analysis: strategies to prevent diversion of opioid substitution treatment medications

Opioid dependence is a complex health condition that usually requires long-term treatment. It tends to be managed with the use of medications in a similar way to other chronic illnesses characterised by possible frequent relapses (McLellan et al., 2000; WHO, 2004), . International guidelines (WHO, 2009; Department of Health, 2007) recommend opioid substitution treatment (OST), such as methadone and buprenorphine, as the main medications for treating opioid dependence. The effectiveness of OST in reducing the risks of overdose and mortality, injecting risk behaviour and illegal opioid use and criminality, and in improving quality of life and health, is well established internationally (Amato et al., 2008; Gowing et al., 2008; Mattick et al., 2008; Lawrinson et al., 2008; Schaub et al., 2010). An estimated 645 000 opioid users received substitution treatment in the European Union in 2014 (683 000 including Norway and Turkey), and numbers have fallen by around 50 000 since 2010. Methadone is the most commonly prescribed opioid substitution drug, received by over two-thirds (70 %) of substitution clients. A further 28 % of clients are treated with buprenorphine-based medication, which is the principal substitution drug in seven countries. Other substances, such as slow-release morphine or diacetylmorphine (heroin), are more rarely prescribed, being received by an estimated 2 % of substitution clients in Europe.
Substitution treatment is regulated by Member States using different types of national law. In almost all countries the admission criteria for substitution treatment programmes are laid down either in national laws or in ministerial decrees or guidelines. The laws usually also define who is permitted to prescribe treatment. These are primarily doctors in treatment centres, though in some countries any doctor or certain trained or accredited doctors may prescribe. Maximum doses are rarely defined by law.
Like any prescription medicines, OST medications can be diverted, despite the existence of legislative controls on their availability. Diversion can be regarded as the inappropriate use of prescribed medicine and has been defined as the unsanctioned supply of regulated pharmaceuticals from legal sources either to the illicit drug market or to a user for whom the drugs were not intended (Larance et al., 2014; Inciardi et al., 2007). Diversion can occur at all points in the drug delivery process: from the original manufacturing site to the wholesale distributor, the physician’s office, the retail pharmacy or the patient (Inciardi et al., 2007). Diversion methods include: the illegal sale and recycling of prescriptions by physicians and pharmacists; the ‘doctor shopping’ phenomenon (Delorme, 2016), whereby individuals consult more than one doctor to obtain multiple prescriptions; theft (including stealing insurance cards to obtain multiple prescriptions), forgery, or alteration of prescriptions by patients; robberies and thefts from manufacturers, distributors, and pharmacies; and thefts of institutional drug supplies (Cicero et al., 2011).
In the last two decades OST diversion has been documented in countries all over the world (Humeniuk et al. 2003, Jenkinson et al. 2005, Cicero et al. 2011, Johnson et al. 2015). Although the diversion of OST medications has been described as a growing problem in recent years, there has been little systematic monitoring or data collection able to quantify the magnitude of the problem. There is also a lack of empirical data that might be used for making regulatory decisions and for developing prescription drug prevention and risk management plans (Cicero et al., 2013). Various reasons have been described in the literature to explain diversion, including (among drug users) attempting to help other users who are not accessing treatment (Havnes 2013, Johnson 2015). Nonetheless, an overview of available studies suggests that the use of diverted substances has been associated with three consequences: fatal and non-fatal overdose; an increased incidence of opioid dependence (particularly in jurisdictions where heroin is scarce); and compromising the public acceptance of treatment programmes (Bell, 2010).
The United States has seen an unprecedented rise in the misuse of prescription opioids and the findings point to an association with overdose deaths and admissions to emergency departments and treatment facilities among people using opioids (Yokell et al., 2011;Weimer et al., 2011; Rosca et al., 2012; Selden et al., 2012; Huang et al., 2013; Richert et al., 2011; Cicero et al., 2011; Wikner et al., 2014).
Longitudinal studies of methadone-related deaths conducted between 2009 and 2012 in the United Kingdom have illustrated the risks of diverted methadone. For example, research has shown that while a significant minority of cases occurred in the in-treatment population, the majority of cases happened in the general population (Corkey, 2013; Ghodse, 2010, 2011, 2012, cit. in Marteau, 2015).
Several studies have found a strong correlation between the levels of medical and non-medical use of prescription opioids (ALICE-RAP, 2013). Non-medical prescription opioid use refers to any use that is not prescribed, or use in a manner other than that intended by the prescriber (Compton et al., 2016). This includes: taking increased doses of the opioid; taking opioids for a longer period of time than intended; taking opioids that were prescribed for another person; obtaining prescriptions under false premises; and obtaining the medication outside of the medical system (ALICE-RAP, 2013). As the medical use of opioids to treat chronic and acute pain has expanded in recent decades, in particular in the United States (Compton et al., 2016) there is concern that this might trigger increased diversion and non-medical use of opioid medications.
In European countries methadone and buprenorphine are the prescription opioids most commonly misused by those who start treatment for drug misuse. Overall, non-medical use of methadone is the most commonly reported opioid addiction other than heroin, followed by buprenorphine. Respectively, these drugs account for 60 % and 30 % of all treatment demands from clients whose primary drug problem relates to opioids other than heroin. In some countries, for example Estonia and Finland, non-heroin opioids now represent the most common form of problem opioid use (EMCDDA, 2016).
Strategies to reduce medication diversion
Certain interventions have been developed with the aim of minimising the diversion of OST. These include the use of misuse-deterrent formulations, supervision of doses for people who are not stable in treatment, the development of clinical prescribing guidelines and education activities to ensure quality of care. Interventions are aimed at patients, physicians and distribution systems. It is likely that a combined approach and treatment plans tailored to patient needs will be most effective, although evidence supporting this is not yet available.
Misuse-deterrent formulations of opioids are being applied in different ways. Opioid formulations have been developed with misuse-deterring properties, such as Suboxone, a combination of buprenorphine and naloxone. Dilution of methadone liquid resulting in large-volume packaging may also discourage injecting.
Educating physicians and patients can be effective in reducing the risk of diversion. Physicians can be educated on safe opioid prescribing, including comprehensive initial assessment and regular monitoring of patients. Patients can be provided with health information and educated on safe use, including information about appropriate storage and disposal of pharmaceuticals that are no longer needed. In a US study a sustained positive change in physician practice behaviours and improved knowledge was found regarding clinical practice behaviours on dosing and setting limits/revising treatment plans following a four-hour course (EMCDDA, 2016).
Electronic medicine dispensers can promote safe opioid prescribing and reduce medical errors, and have been implemented in the United States and some other countries. A small Finnish study evaluating the use of electronic medical dispensers in 37 OST patients found some evidence that electronic dispensers had prevented diversion of buprenorphine-naloxone. Most patients felt it was safer to store take-home doses in electronic dispensers than in paper sachets (Uosukainen et al., 2013).
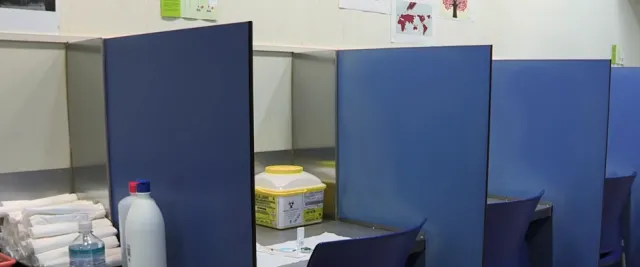
Supervision of OST dosing is likely to reduce the diversion of OST. Clinical guidelines that cover methadone and buprenorphine treatment in the United Kingdom, and in Canada (Department of Health, 2007; CAMH, 2011) recommend initial supervision of OST. Subsequent suitability for unsupervised dosing is based on assessment of a client’s social functioning (employment, housing), on cessation of regular injecting, on not presenting intoxicated for dosing and on low levels of ongoing drug misuse (confirmed by urine toxicology). In addition, guidelines produced by the World Health Organization on the combination of specific pharmacological and psychosocial interventions (WHO, 2009) recommend supervision of dosing for both methadone and buprenorphine to reduce the risk of diversion in opioid dependents, especially at the start of treatment; take-away doses may be provided when patients are considered stable and the risk of diversion is low.
A study of dependence treatment centres in Italy found that: take-home doses in the context of a behavioural contingency management programme did not increase unlawful behaviour; and patients in a non-contingent take-home programme were over six times more likely to sell their methadone on the black market than those in a six days per week supervised daily consumption programme (Gerra et al., 2011). A study in England and Scotland looked at mortality rates for methadone-related overdoses during a 16-year period. It found that a reduction of overdoses corresponded to the introduction of facilities for supervised consumption of methadone (Strang, 2010).
Monitoring patients is another way to reduce diversion. Clinical guidelines recommend the surveillance and monitoring of patients in OST with the aim of reducing the risk of medication diversion (see ‘Facts and figures’). Such monitoring may include toxicology screening/drug testing, pill counts, unannounced monitoring/random call-backs (especially for those with extended take-home doses) and supervised ingestion (Martin et al., 2014).
Diversion control systems target the wider distribution system. A US review on existing drug diversion control systems (Deyo, 2014) distinguished two basic goals: first, to limit access to the controlled substances only to those with a legitimate need for access; and second, to establish, through records and reporting, the ability to track and identify instances in which the access controls are compromised (Deyo, 2014).
In the United States, since 2005, databases have been established in 38 states that collect information on the prescriber, pharmacy, product name, concentration, dose and amount of controlled substance dispensed (Prescription Drug Monitoring Programmes (PDMP)). Similar programmes exist in Australia and some parts of Europe. Although some studies have suggested that these programmes have a substantial impact on reducing the supply of monitored drugs and the rates of drug misuse, their quality is variable, and their success relies on a variety of factors.
Current evaluation findings
To date, it is not yet clear which of the approaches outlined above are most effective in preventing the diversion of OST medications. Most interventions have occurred on an ad hoc basis, and commentators have emphasised the need for systematic evaluations of their effects on reducing diversion in the interest of evidence-based policy and public health. It also remains to be established whether policies contribute to a reduction of diversion when they are included in an integrated drug control system or whether certain strategies constitute cost-effective stand-alone interventions.
A summary of evidence is critical in order to support informed decision-making on which elements of anti-diversion systems are effective in reducing opioid diversion, and which require further research.
AN EMCDDA analysis identified six studies evaluating at different levels some strategies for the prevention and/or reduction of OST diversions (see table below). These studies addressed various targets, such as: patients, physicians or the system of OST distribution.
| Target group | Possible strategies to reduce / control diversion | Synthesis of evidence | References |
|---|---|---|---|
| Patients | Misuse-deterrent drug formulations | Significantly fewer methadone clients reported diversion compared to buprenorphine-naloxone tablet clients. Addition of naloxone reduces, but does not abolish, diversion. Clinicians need to employ patient selection for prescribing of doses without observation, and monitor patients regularly, rather than relying solely upon the formulation of the medication to minimise risk. | Larance et al, 2014 (Australia; N=543 patients) Bell., 2011 (United Kingdom, Australia, United States, France; N= not applicable) |
| Patients | Health education, including safe storage | Doctors prescribing opioids for pain treatment should be trained on how to regularly monitor their patients. | Hahn, 2011 |
| Patients | Supervision of OST dosing | Early non-contingent take-home patients were over six times more likely to sell their medication or part of it on the black market once or twice a week. Introduction of supervised methadone dosing was followed by substantial declines in deaths related to overdose of methadone (Scotland and England). | Gerra, 2011 (Italy; N=300 patients) Strang, 2010 (Scotland, England death records 1993–2008; N=5 624 death records) |
| Patients | Monitoring patients, e.g. toxicology tests, pill counts, unannounced monitoring and observed ingestion | Some recommendations exist for the identification of ‘red flag’ behaviours that indicate possible diversion. In these cases: preference for misuse-deterrent formulations, toxicology, examination of injecting sites and child protection assessment, pill counts, observed ingestion and advise patients regarding appropriate medication storage. | Martin, 2014 (Australia; N= not applicable) Bell, 2011 (United Kingdom, Australia, United States, France; N= not applicable) |
| Physicians | Continuing medical education including safe opioid (buprenorphine) prescribing, initial patient assessment and monitoring for physicians in office-based opioid dependence treatment | Positive change in physician practice behaviours and improved knowledge that was sustained. | Lofwall, 2011 (US; N=311 physicians) |
| Physicians | Electronic medicine dispensers (EMD) | The use of EMDs provided a feasible method for improving the safe storage of take-home doses of buprenorphine- naloxone. | Uosukainen 2013 (Finland; N=56) |
| System of distribution | To limit access to the controlled substances only to those with a legitimate need for access; to establish the ability to track and identify instances in which the access controls are compromised | Six systems described, of varying utility as reported by users; monitoring programmes exist in 44 US states and some other countries, their quality is variable, and their effects on public health are being explored. Clinical guidelines and clinical audit to enhance compliance with guidelines are helpful in maintaining the quality and integrity of the treatment system, and can contribute to keeping diversion within acceptable levels. Medication management system should ensure that medications are available to those who need it, while monitoring for and preventing possible diversion. | Deyo, 2014 (Prescription monitoring systems in 44 states) Bell, 2011 (UK, Australia, US, France; N= not applicable) UNODC, 2011 (UNODC discussion paper) |
Conclusion
It is difficult to estimate the extent of diversion from opioid substitution treatment in Europe. Nonetheless, given the important role substitution treatment has in Europe it is critical that a more systematic understanding of what is effective is used to support treatment systems. Current evidence suggests that the risks of diversion of OST medications from treatment settings can be reduced by the application of clinical standards and guidelines for appropriate dosing, supervision of doses for people who are not stable in treatment, for identification of patients ready for unobserved doses and education activities to ensure quality of care. Other strategies include the use of alternative formulations and dilution of take-away OST doses.
There is a need for more systematic evaluation of the different strategies that are being used to reduce diversion. To support, this observational studies or randomised controlled trials that systematically compare the different strategies should be used to identify the most effective interventions. This will allow the development of best practices that can be more widely rolled out. A summary of evidence is needed to support informed decision-making on policies for diversion and to define which elements of diversion systems are effective in reducing opioid diversion.
Footnotes
(1) Footnote 1
(2) Footnote 2
References
ALICE RAP (Addictions and Lifestyles in Contemporary Europe – Reframing Addictions Project) (2013), Prescription opioids and public health in the European Union’, Policy Brief 4.
Amato, L., Minozzi, S., Davoli, M., Vecchi, S., Ferri, M., Mayet, S. (2008), ‘Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification’, Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD005031.
Bell, J. (2010), ‘The global diversion of pharmaceutical drugs: Opiate treatment and the diversion of pharmaceutical opiates: A clinician’s perspective’, Addiction 105(9), pp. 1531–7.
Brisacier, A. C. and Collin, C. (2014), ‘Opioid substitution treatments in France: Recent data’, Tendances 94, OFDT (French Monitoring Centre for Drugs and Drug Addiction).
Centre for Addiction and Mental Health (CAMH) (2011), Buprenorphine Guideline for treatment of Opioid Dependence. Available at: www.cpso.on.ca/uploadedFiles/policies/guidelines/office/buprenorphine_n…
Cicero, T. J., Kurtz, S. P., Surratt, H. L., et al. (2011) ‘Multiple determinants of specific modes of prescription opioid diversion’, Journal of Drug Issues 41(2), pp. 283–304.
Cicero, T. J., Ellis, M. S., Surratt, H. L., Kurtz, S. P. (2013), ‘Factors influencing the selection of hydrocodone and oxycodone as primary opioids in substance abusers seeking treatment in the United States’, Pain®, 154(12), pp. 2639–48.
Compton, W. M., Jones, C. M., Baldwin, G. T. (2016), ‘Relationship between Nonmedical Prescription-Opioid Use and Heroin Use’, New England Journal of Medicine, 374(2), pp. 154–63.
Dart, R. C., Surratt, H. L., Cicero, T. J., et al. (2015), ‘Trends in opioid analgesic abuse and mortality in the United States’, The New England Journal of Medicine 372(3), pp. 241–8.
Delorme, J., Chenaf, C., Kabore, J.-L., et al. (2016), ‘Incidence of high dosage buprenorphine and methadone shopping behavior in a retrospective cohort of opioid-maintained patients in France’, Drug and Alcohol Dependence 162, pp. 99–106.
Department of Health England and the devolved administrations (2007), Drug Misuse and Dependence: UK Guidelines on Clinical Management. Retrieved from http://www.nta.nhs.uk/uploads/clinical_guidelines_2007.pdf
Deyo, R. A., Irvine, J. M., Millet, L. M., Beran, T., O’Kane, N., Wright, D. A., McCarty, D. (2013), ‘Measures such as interstate cooperation would improve the efficacy of programs to track controlled drug prescriptions’, Health Affairs, pp. 10-1377.
EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2016), European Drug Report 2016: Trends and Developments, Publications Office of the European Union, Luxembourg.
FDA (Food and Drug Administration) (2015), Abuse-deterrent opioids — evaluation and labeling: Guidance for industry, FDA, New Hampshire.
Gerra, G., Saenz, E., Busse, A., Maremmani, I., Ciccocioppo, R., Zaimovic, A., Somaini, L. (2011), ‘Supervised daily consumption, contingent take-home incentive and non-contingent take-home in methadone maintenance’, Progress in Neuro-Psychopharmacology and Biological Psychiatry, 35(2), pp. 483–9.
Gowing, L., Farrell, M., Bornemann, R., Sullivan, L.E., Ali, R. (2008), ‘Substitution treatment of injecting opioid users for prevention of HIV infection’, Cochrane Database of Systematic Reviews 2008, Issue 2. Art. No.: CD004145.
Hahn, K. L. (2011) ‘Strategies to prevent opioid misuse, abuse, and diversion that may also reduce the associated costs’, American Health and Drug Benefits 4(2), pp. 107–14.
Havnes, I. A., Clausen, T., Middelthon, A. L. (2013), ‘Diversion of methadone or buprenorphine: harm versus helping’, Harm Reduction Journal, 10(1), p. 1.
Huang, C.L., Lee, C.W. (2013), ‘Factors associated with mortality among heroin users after seeking treatment with methadone: a population-based cohort study in Taiwan’, Journal of Substance Abuse Treatment 44(3), pp. 295–300.
Humeniuk, R., Ali, R., McGregor ,C., Darke, S. (2003), ‘Prevalence and correlates of intraveneous methadone syrup administration in Adelaide Australia’, Addiction 98, pp. 413–8.
Inciardi, J. A., Surratt, H. L., Lugo, Y. and Cicero, T. J. (2007), ‘The diversion of prescription opioid analgesics’, Law Enforcement Executive Forum November, 7(7), pp. 127–41.
Jenkinson, R., Clark, N.C., Fry, C.L., Dobbin, M. (2005), ‘Buprenorphine diversion and injection in Melbourne, Australia: An emerging issue?’, Addiction 100, pp. 197–205.
Johnson, B. Richert, T. (2015), ‘Diversion of methadone and buprenorphine by patients in opioid substitution treatment in Sweden: Prevalence estimates and risk factors’, International Journal of Drug Policy 26(2), pp. 183–90.
Larance, B., Degenhardt, L., Lintzeris, N., Winstock, A. and Mattick, R. (2014), ‘Definitions related to the use of pharmaceutical opioids: Extramedical use, diversion, non-adherence and aberrant medication-related behaviours’, Drug and Alcohol Review 30(3), pp. 236–45.
Lawrinson, P., Ali, R., Buavirat, A.et al. (2008), ‘Key findings from WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS’, Addiction 103, pp. 1484–92.
Lofwall, M. R., Walsh, S. L. (2013), ‘A review of buprenorphine diversion and misuse: the current evidence base and experiences from around the world’, Journal of Addiction Medicine 8(5), pp. 315–26.
Marteau, D., McDonald, R. and Patel, K. (2015), ‘The relative risk of fatal poisoning by methadone or buprenorphine within the wider population of England and Wales’, BMJ Open 5(5): e007629.
Martin, J. (2014), ‘Adherence, diversion and misuse of sublingual buprenorphine’, PCSS Online http://pcssmat.org/wp-content/uploads/2014/02/PCSS-MATGuidanceAdherence-diversion-bup.Martin.pdf
Mattick, R.P. et al. (2014), ‘Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence’, Cochrane Database Syst Rev. 6, p. 2.
McLellan, A. T., Lewis, D. C., O'Brien, C. P., Kleber, H. D. (2000), ‚Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation’, Jama, 284(13), pp. 1689–95.
Richert, T., Johnson, B. (2013), ‘Illicit use of methadone and buprenorphine among adolescents and young adults in Sweden’, Harm Reduction Journal 10, p. 27.
Rosca, P., Haklai, Z., Goldberger, N., Zohar, P., Margolis, A., Ponizovsky, A.M. (2012), ‘Mortality and causes of death among users of methadone maintenance treatment in Israel, 1999-2008’, Drug and Alcohol Dependence 125(1-2), pp. 160–3. Erratum in: Drug and Alcohol Dependence 2012 Nov 1, p. 126, 1-2, p. 277.
Schaub, M., Chtenguelov, V., Subata, E. et al. (2010), ‘Feasibility of buprenorphine and methadone maintenance programmes among users of homemade opioids in Ukraine’, International Journal of Drug Policy 21(3), pp. 229–33.
Seldén, T., Ahlner, J., Druid, H., Kronstrand, R. (2012), ‘Toxicological and pathological findings in a series of buprenorphine related deaths. Possible risk factors for fatal outcome’, Forensic Science International 220(1-3), pp.284–90.
Strang, J., Hall, W., Hickman, M., Bird, S. M. (2010), ‘Impact of supervision of methadone consumption on deaths related to methadone overdose (1993-2008): analyses using OD4 index in England and Scotland’, BMJ 341, c4851.
Uosukainen, H., Pentikäinen, H., Tacke, U. (2013), ’The effect of an electronic medicine dispenser on diversion of buprenorphine-naloxone—experience from a medium-sized Finnish city’, Journal of Substance Abuse Treatment 45(1), pp. 143–7.
UNODC (United Nations Office on Drugs and Crime) (2011), The non-medical use of prescription drugs: Policy direction issues, UNODC, Vienna.
Weimer, M.B., Korthuis, P.T., Behonick, G.S., Wunsch, M.J. (2011), ‘The source of methadone in overdose deaths in Western Virginia in 2004’, Journal of Addiction Medicine 5(3), pp. 188–202.
Wikner, B.N., Ohman, I., Seldén, T., Druid, H., Brandt, L., Kieler, H. (2014), ‘Opioid-related mortality and filled prescriptions for buprenorphine and methadone’, Drug and Alcohol Review doi:10.1111/dar.12143.
World Health Organization (2004), Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention, position paper World Health Organization, United Nations Office on Drugs and Crime, UNAIDS.
World Health Organization (2009), Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence, World Health Organization, Geneva.
Yokell, M.A., Zaller, N.D., Green, T.C., Rich, J.D. (2011), ‘Buprenorphine and buprenorphine/naloxone diversion, misuse, and illicit use: an international review’, Current Drug Abuse Reviews 4(1), pp. 28–41.
Motion graphic: opioid substitution treatment explained
Terms and definitions
Definitions
Opioid substitution therapy (OST) (see the video) indicates an intervention in which patients who are dependent on fast-acting opioids (such as heroin) are administered slow-acting opioids instead (such as methadone and buprenorphine). The treatment is described using a range of terms, including ‘substitution’, ‘maintenance’, ‘agonist’ and ‘pharmacologically assisted’. The term OST has limitations because it does not describe the nature of the medications involved, which do not necessarily have substitutive effects for illicit opioids, but may instead reduce cravings and support the control of addictive behaviour.
Diversion of a medicine is defined as the intentional transfer of a controlled drug from legitimate distribution and dispensing into illegal channels.
Misuse is defined as the use of a medication other than as directed or as indicated, whether wilful or unintentional, and whether it results in harm or not.
What do the guidelines say?
Most of the available guidelines on the treatment of opioid dependence agree on the importance of providing access to opioid substitution therapy and suggest that the professional responsible for the prescription should assess the possible risks of diversion on a case-by-case basis.
Some examples of guidelines have been selected from the inventory of the Best practice portal.
The World Health Organization’s Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence (2009) address the risks of diversion in various parts of the guidelines and in some specific recommendations. In particular, they recommend offering medication take-home doses when the dose itself and the social situation is stable and there is a low risk of diversion for illegitimate purposes.
The same recommendation suggests monitoring the safety of the treatment service, including the extent of medication diversion.
The recommendations for the treatment of individual patients include:
- supervision of methadone and buprenorphine doses in the early phase of treatment (the recommendation is strong for the panel developing the guidelines but based on a low level of evidence);
- take-away doses may be provided for patients when the benefits of reduced frequency of attendance are considered to outweigh the risk of diversion, subject to regular review (the recommendation is strong for the panel developing the guidelines but based on a low level of evidence).
The Canadian guidelines on buprenorphine/naloxone for opioid dependence (2011) recommend that, when making decisions regarding the provision of take-home doses of buprenorphine/naloxone, providers should use a clinical risk stratification strategy (as described in the clinical considerations) that aims to support patient autonomy while at the same time respecting patient and public safety. (Level III, Grade A, meaning that the level of evidence is low but the panel agrees on a strong recommendation.)
At the European level, for example the European Centre for Disease Prevention and Control (ECDC)–EMCDDA joint Guidelines on prevention and control of infectious diseases among people who inject drugs mention that ‘opioid substitution medications can be dispensed in clinics, in specialised centres in the community or in pharmacies. In all settings, the direct supervision of the patient taking the medications can prevent diversion of drugs to the illicit market. However, take-home doses allow patients to follow family- or work-related obligations and lead a more “normal” life. For all undergoing such treatment, regular medical examinations are an essential requirement’
References
- CAMH (2011) Buprenorphine Guideline for treatment of Opioid Dependence
- ECDC and EMCDDA guidance. Prevention and control of infectious diseases among people who inject drugs EMCDDA/ECDC, Stockholm, October 2011
- World Health Organization (2009), Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence, World Health Organization, Geneva.
The evidence for opioid substitution treatment in Europe

Substitution treatment, typically combined with psychosocial interventions, is the most common treatment for opioid dependence. This approach is supported by the available evidence, with positive outcomes found in respect of treatment retention, reduced illicit opioid use, reported risk behaviour, and reductions in drug-related harms and mortality.
Evidence base
OST, combined with psychosocial support, helps patients stay in treatment and reduces use and mortality. It also has a positive impact on the mental health of patients. Methadone and buprenorphine are the recommended pharmacological treatments. Taking into account clinical practice, methadone is superior to buprenorphine in retaining people in treatment, particularly in the first weeks, and equally suppresses illicit opioid use.
There is a strong evidence base for the use of OST, including the following studies, and in the last update of the Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence (WHO, 2009). Methadone substitution treatment was found in a systematic review of three randomised controlled trials (RCTs) (N=505) (WHO, 2009) to be more effective than opioid withdrawal, followed by placebo, in increasing retention in treatment and reducing illicit opioid use. Observational studies found the mortality rate in methadone treatment to be approximately one-third the rate out of treatment. Methadone was found in one RCT (N=253) to reduce the risk of HIV infection by approximately 50 % and a similar reduction in seroconversion rates was found in three observational studies (N=43.035) (RR 0.36, 95 % CI 0.19 to 0.66) when compared to withdrawal or no treatment.
Buprenorphine substitution treatment was found to be more effective than placebo in a synthesis of evidence (WHO, 2009). More recently, in a systematic review (Mattick et al., 2014) it was found to improve retention in treatment and reduce the number of morphine-positive urines only at high doses.
Methadone treatment plus psychosocial intervention compared with methadone treatment only was found in a systematic review of three studies (N=388), to be more effective in reducing heroin use (RR 0.69, 95 % CI 0.53 to 0.91) (WHO, 2009). Combined psychosocial (contingency management, community reinforcement, psychotherapeutic counselling and family therapy) and pharmacological assistance have been found to be effective in a systematic review of five randomised control trials (N=184 participants) in increasing rates of completion of treatment and reducing rates of relapse at follow-up (WHO, 2009).
References
ALICE RAP (Addictions and Lifestyles in Contemporary Europe – Reframing Addictions Project) (2013), Prescription opioids and public health in the European Union’, Policy Brief 4.
Amato, L., Minozzi, S., Davoli, M., Vecchi, S., Ferri, M., Mayet, S. (2008), ‘Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification’, Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD005031.
Bell, J. (2010), ‘The global diversion of pharmaceutical drugs: Opiate treatment and the diversion of pharmaceutical opiates: A clinician’s perspective’, Addiction 105(9), pp. 1531–7.
Brisacier, A. C. and Collin, C. (2014), ‘Opioid substitution treatments in France: Recent data’, Tendances 94, OFDT (French Monitoring Centre for Drugs and Drug Addiction).
Centre for Addiction and Mental Health (CAMH) (2011), Buprenorphine Guideline for treatment of Opioid Dependence. Available at: www.cpso.on.ca/uploadedFiles/policies/guidelines/office/buprenorphine_n…
Cicero, T. J., Kurtz, S. P., Surratt, H. L., et al. (2011) ‘Multiple determinants of specific modes of prescription opioid diversion’, Journal of Drug Issues 41(2), pp. 283–304.
Cicero, T. J., Ellis, M. S., Surratt, H. L., Kurtz, S. P. (2013), ‘Factors influencing the selection of hydrocodone and oxycodone as primary opioids in substance abusers seeking treatment in the United States’, Pain®, 154(12), pp. 2639–48.
Compton, W. M., Jones, C. M., Baldwin, G. T. (2016), ‘Relationship between Nonmedical Prescription-Opioid Use and Heroin Use’, New England Journal of Medicine, 374(2), pp. 154–63.
Dart, R. C., Surratt, H. L., Cicero, T. J., et al. (2015), ‘Trends in opioid analgesic abuse and mortality in the United States’, The New England Journal of Medicine 372(3), pp. 241–8.
Delorme, J., Chenaf, C., Kabore, J.-L., et al. (2016), ‘Incidence of high dosage buprenorphine and methadone shopping behavior in a retrospective cohort of opioid-maintained patients in France’, Drug and Alcohol Dependence 162, pp. 99–106.
Department of Health England and the devolved administrations (2007), Drug Misuse and Dependence: UK Guidelines on Clinical Management. Retrieved from http://www.nta.nhs.uk/uploads/clinical_guidelines_2007.pdf
Deyo, R. A., Irvine, J. M., Millet, L. M., Beran, T., O’Kane, N., Wright, D. A., McCarty, D. (2013), ‘Measures such as interstate cooperation would improve the efficacy of programs to track controlled drug prescriptions’, Health Affairs, pp. 10-1377.
EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2016), European Drug Report 2016: Trends and Developments, Publications Office of the European Union, Luxembourg.
FDA (Food and Drug Administration) (2015), Abuse-deterrent opioids — evaluation and labeling: Guidance for industry, FDA, New Hampshire.
Gerra, G., Saenz, E., Busse, A., Maremmani, I., Ciccocioppo, R., Zaimovic, A., Somaini, L. (2011), ‘Supervised daily consumption, contingent take-home incentive and non-contingent take-home in methadone maintenance’, Progress in Neuro-Psychopharmacology and Biological Psychiatry, 35(2), pp. 483–9.
Gowing, L., Farrell, M., Bornemann, R., Sullivan, L.E., Ali, R. (2008), ‘Substitution treatment of injecting opioid users for prevention of HIV infection’, Cochrane Database of Systematic Reviews 2008, Issue 2. Art. No.: CD004145.
Hahn, K. L. (2011) ‘Strategies to prevent opioid misuse, abuse, and diversion that may also reduce the associated costs’, American Health and Drug Benefits 4(2), pp. 107–14.
Havnes, I. A., Clausen, T., Middelthon, A. L. (2013), ‘Diversion of methadone or buprenorphine: harm versus helping’, Harm Reduction Journal, 10(1), p. 1.
Huang, C.L., Lee, C.W. (2013), ‘Factors associated with mortality among heroin users after seeking treatment with methadone: a population-based cohort study in Taiwan’, Journal of Substance Abuse Treatment 44(3), pp. 295–300.
Humeniuk, R., Ali, R., McGregor ,C., Darke, S. (2003), ‘Prevalence and correlates of intraveneous methadone syrup administration in Adelaide Australia’, Addiction 98, pp. 413–8.
Inciardi, J. A., Surratt, H. L., Lugo, Y. and Cicero, T. J. (2007), ‘The diversion of prescription opioid analgesics’, Law Enforcement Executive Forum November, 7(7), pp. 127–41.
Jenkinson, R., Clark, N.C., Fry, C.L., Dobbin, M. (2005), ‘Buprenorphine diversion and injection in Melbourne, Australia: An emerging issue?’, Addiction 100, pp. 197–205.
Johnson, B. Richert, T. (2015), ‘Diversion of methadone and buprenorphine by patients in opioid substitution treatment in Sweden: Prevalence estimates and risk factors’, International Journal of Drug Policy 26(2), pp. 183–90.
Larance, B., Degenhardt, L., Lintzeris, N., Winstock, A. and Mattick, R. (2014), ‘Definitions related to the use of pharmaceutical opioids: Extramedical use, diversion, non-adherence and aberrant medication-related behaviours’, Drug and Alcohol Review 30(3), pp. 236–45.
Lawrinson, P., Ali, R., Buavirat, A.et al. (2008), ‘Key findings from WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS’, Addiction 103, pp. 1484–92.
Lofwall, M. R., Walsh, S. L. (2013), ‘A review of buprenorphine diversion and misuse: the current evidence base and experiences from around the world’, Journal of Addiction Medicine 8(5), pp. 315–26.
Marteau, D., McDonald, R. and Patel, K. (2015), ‘The relative risk of fatal poisoning by methadone or buprenorphine within the wider population of England and Wales’, BMJ Open 5(5): e007629.
Martin, J. (2014), ‘Adherence, diversion and misuse of sublingual buprenorphine’, PCSS Online http://pcssmat.org/wp-content/uploads/2014/02/PCSS-MATGuidanceAdherence-diversion-bup.Martin.pdf
Mattick, R.P. et al. (2014), ‘Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence’, Cochrane Database Syst Rev. 6, p. 2.
McLellan, A. T., Lewis, D. C., O'Brien, C. P., Kleber, H. D. (2000), ‚Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation’, Jama, 284(13), pp. 1689–95.
Richert, T., Johnson, B. (2013), ‘Illicit use of methadone and buprenorphine among adolescents and young adults in Sweden’, Harm Reduction Journal 10, p. 27.
Rosca, P., Haklai, Z., Goldberger, N., Zohar, P., Margolis, A., Ponizovsky, A.M. (2012), ‘Mortality and causes of death among users of methadone maintenance treatment in Israel, 1999-2008’, Drug and Alcohol Dependence 125(1-2), pp. 160–3. Erratum in: Drug and Alcohol Dependence 2012 Nov 1, p. 126, 1-2, p. 277.
Schaub, M., Chtenguelov, V., Subata, E. et al. (2010), ‘Feasibility of buprenorphine and methadone maintenance programmes among users of homemade opioids in Ukraine’, International Journal of Drug Policy 21(3), pp. 229–33.
Seldén, T., Ahlner, J., Druid, H., Kronstrand, R. (2012), ‘Toxicological and pathological findings in a series of buprenorphine related deaths. Possible risk factors for fatal outcome’, Forensic Science International 220(1-3), pp.284–90.
Strang, J., Hall, W., Hickman, M., Bird, S. M. (2010), ‘Impact of supervision of methadone consumption on deaths related to methadone overdose (1993-2008): analyses using OD4 index in England and Scotland’, BMJ 341, c4851.
Uosukainen, H., Pentikäinen, H., Tacke, U. (2013), ’The effect of an electronic medicine dispenser on diversion of buprenorphine-naloxone—experience from a medium-sized Finnish city’, Journal of Substance Abuse Treatment 45(1), pp. 143–7.
UNODC (United Nations Office on Drugs and Crime) (2011), The non-medical use of prescription drugs: Policy direction issues, UNODC, Vienna.
Weimer, M.B., Korthuis, P.T., Behonick, G.S., Wunsch, M.J. (2011), ‘The source of methadone in overdose deaths in Western Virginia in 2004’, Journal of Addiction Medicine 5(3), pp. 188–202.
Wikner, B.N., Ohman, I., Seldén, T., Druid, H., Brandt, L., Kieler, H. (2014), ‘Opioid-related mortality and filled prescriptions for buprenorphine and methadone’, Drug and Alcohol Review doi:10.1111/dar.12143.
World Health Organization (2004), Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention, position paper World Health Organization, United Nations Office on Drugs and Crime, UNAIDS.
World Health Organization (2009), Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence, World Health Organization, Geneva.
Yokell, M.A., Zaller, N.D., Green, T.C., Rich, J.D. (2011), ‘Buprenorphine and buprenorphine/naloxone diversion, misuse, and illicit use: an international review’, Current Drug Abuse Reviews 4(1), pp. 28–41.
EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2016) ‘Best practice portal: Treatment options for opioid users’, EMCDDA, Lisbon.
EMCDDA (2016), ‘Best practice in drug interventions: Treatment for opioid users’, EMCDDA, Lisbon.
References
Mattick, R.P., Breen, C., Kimber, J., Davoli, M.(2014), ‘Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence’, Cochrane Database Syst Rev. 6, p.2.
World Health Organization (2009), Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence, World Health Organization, Geneva.
Find out more
Further reading
EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2016) ‘Best practice portal: Treatment options for opioid users’, EMCDDA, Lisbon.
EMCDDA (2016), ‘Best practice in drug interventions: Treatment for opioid users’, EMCDDA, Lisbon.
References
Mattick, R.P., Breen, C., Kimber, J., Davoli, M.(2014), ‘Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence’, Cochrane Database Syst Rev. 6, p.2.
World Health Organization (2009), Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence, World Health Organization, Geneva.