Perspectives on drugs: emergency health consequences of cocaine use in Europe
Introduction
Emergency health consequences of cocaine use in Europe

Every year, several thousands of cocaine-related emergencies are reported in Europe, along with hundreds of cocaine-related deaths. The types of cocaine-related problems reported are wide-ranging and the relatively high prevalence of cocaine use in the general population means that there is likely to be a significant impact on overall public health.
The last decade has seen cocaine establish itself as the most commonly used illicit stimulant drug in Europe, with an estimated 2.5 million young adults (aged 15–34) using the drug in the last year. Overall, powder cocaine is the most common form of the drug used, and high levels of use tend to be concentrated in a relatively small number of western European countries (e.g. Denmark, Spain, Ireland, Italy, the United Kingdom). Crack cocaine use and its associated problems, is reported by a limited number of countries, and often overlaps with the use of heroin and other substances. Although many users of cocaine will not experience problems, a minority will suffer acute adverse effects that may result in them receiving help from emergency services.
Acute emergencies: a window on cocaine-related problems
A recent EMCDDA study provided a first overview of cocaine-related emergency episodes reported in Europe. The data were mostly collected retrospectively, from on-going monitoring systems in place in hospitals, at either local or national level. The results highlight the fact that countries were using a range of different definitions and data sources to monitor cocaine-related emergencies at the national level (Mena et al., 2012). Overall, however, around two-thirds or more of all the reported cases involved males, although there was variation between countries. Building on the study methodology, countries have provided updates with their most recent data on cocaine episodes. According to this, Spain reported the highest number of emergency cases (2 386 in 2011), followed by the United Kingdom (2 247 hospital discharges in 2010/2011), Italy (1 898 hospital admissions in 2009), the Netherlands (896 hospital admissions in 2011) and Denmark (150 patients registered at emergency departments in 2011). Data is also available for the UK (England) with 662 hospital discharges reported in 2011/2012). Although the proportion of all drug-related hospital emergency episodes that are related to cocaine varies between countries, depending to a large extent on the prevalence of cocaine use, in Spain, for example, half of all drug-related hospital emergencies in 2010 were reportedly cocaine-related.
The numbers of cocaine-related problems reported in Europe are, for a number of reasons, likely to be underestimated. One reason for this is that cases may be coded according to the symptoms (e.g. chest pain, convulsions, stroke etc.) rather than as being due to cocaine. In addition, in some countries, hospital data are only available for patients who are admitted (inpatient stay). A study in one London hospital found that around 50% of those who presented to the emergency department with cocaine (and all recreational drug-related) toxicity were admitted to hospital. The other 50% of cases who are discharged were not captured by the system. In this case the hospital inpatient data would grossly underestimate the overall prevalence of patients presenting with acute cocaine-related toxicity (Wood, 2010).
Trends in cocaine-related emergencies
Both the differences in type of data source used to monitor cocaine-related emergency episodes and limitations of the data make comparison between and even within countries difficult. Nevertheless, as the case definitions and collection systems have remained unchanged over time in most countries; this allows analysis of time trends. Taking a long-term perspective, there has been a two- to three-fold increase in the number of cocaine-related emergency episodes reported since the end of the 1990s in some European countries. In Spain and the United Kingdom, these increases appear to have peaked around 2007–08 and have subsequently dropped. The overall trend is consistent with changing prevalence of use among the young population; with rates of cocaine-related deaths; and with the number of people entering treatment with cocaine as the primary drug. The picture varies between countries, however (see Figures 1–4 on this page).

Acute cocaine-related health problems
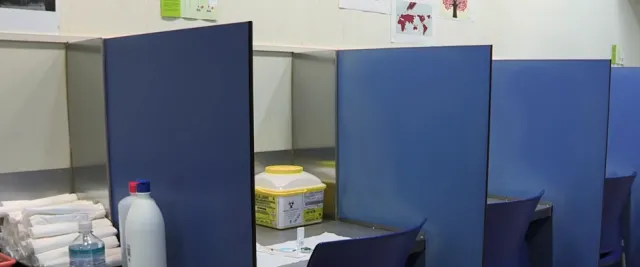
Hospital emergency admissions related to cocaine use involve clients presenting with a range of physical and neuropsychiatric adverse effects (see 'A vignette of typical victims of a cocaine-related emergency in northern Italy').
Symptoms associated with acute cocaine-related cases commonly include agitation, anxiety, aggression and seizures. A further acute and potentially life-threatening complication can be hyperthermia (a very elevated body temperature). Acute psychiatric symptoms can include suicidal thoughts and psychosis. The cardiac effects of cocaine may range from tachycardia (fast heart rate), hypertension (high blood pressure), arrhythmias (abnormal heart rhythm) to chest pain due to acute coronary syndrome and myocardial infarction. Chronic cocaine use has been associated with an increased risk of coronary artery disease, cardiomyopathy (deterioration in heart muscle function) and stroke (Dinis-Oliveira, 2012).
Cocaine use and alcohol use, in particular heavy episodic drinking, are often associated, and this may be factor in some emergency admissions linked with violence or traffic accidents (EMCDDA, 2012).
Cocaine-related deaths: under-reported and underestimated
While many cocaine-related emergencies will not result in serious or long-term health problems, at the other end of the scale some European countries do report significant numbers of cocaine-related deaths. It is likely that many deaths go unreported and that overall cocaine-related mortality is underestimated. Also the type of cases reported, the recording practices and the sources used vary considerably between countries. Nevertheless, in Europe, the majority of cocaine-related deaths are reported in Spain (almost 300 cases of cocaine-related deaths in 2010) and the United Kingdom (152 cases with ‘mentions’ of cocaine on the death certificate in 2011), also mirroring the relatively high prevalence of use in these countries. In addition, some 20 to 50 cases are reported annually from other European countries (Corkery 2012).
Recent studies suggest that mortality can be four to eight times higher among cocaine users than age and sex peers in the general population (Degenhardt et al., 2011; de la Fuente et al., 2013).Most of these cocaine-related deaths are among young males, many of whom have used cocaine with opioids and a range of other drugs. Most cases involved overdose, but a minority die of less specific causes, for example cardiovascular problems. In some cases, the concomitant use of other drugs makes it difficult to establish a causal link with cocaine.
Conclusion and public health implications
There is no doubt that the use of cocaine currently places a considerable burden on emergency services in Europe; however, the presentation of cocaine users at emergency departments also offers an opportunity for services to make contact with a group that may otherwise be hard to reach. There is clearly some potential for early identification, assessment and referral opportunities for many cocaine users who might otherwise be overlooked. The benefit of using hospital emergency data for monitoring acute problems associated with cocaine use is relatively clear and further work is needed to harmonise and improve this data set. In future, it will also be important to explore how this data source might be used to monitor acute toxicity and health problems associated with the use of other drugs, including amphetamines, prescription opioids and new psychoactive substances.
References
- Mena, G., Giraudon, I., Alvarez, E., Corkery, J. M., Matias, J. et al. (2013), 'Cocaine-related health emergencies in Europe: a review of sources of information, trends and implications for service development', European Addiction Research 19(2), pp. 74–81.
- Wood, D. M. and Dargan, P. I. (2010), ‘Putting cocaine use and cocaine-associated cardiac arrhythmias into epidemiological and clinical perspective’, British Journal of Clinical Pharmacology 69(5), pp. 443–447.
- Dinis-Oliveira, R. J., Carvalho, F., Duarte, J. A., Proenca, J. B., Santos, A. and Magalhaes, T. (2012), 'Clinical and forensic signs related to cocaine abuse', Current Drug Abuse Review 5(1), pp. 64–83.
- EMCDDA (2012), Driving under the influence of drugs, alcohol and medicines in Europe: findings from the DRUID project, Publications Office of the European Union, Luxembourg, pp. 1–57.
- Corkery J.M. (2012), ‘Analysis of the data sources, numbers and characteristics of cocaine-related DRD cases reported in Special Mortality Registries, or eventually in General Mortality Registries (GMR) when necessary’, pp. 28. Available with appendices from https://www.emcdda.europa.eu/themes/key-indicators/drd
- Degenhardt, L., Singleton, J., Calabria, B., McLaren, J., Kerr, T., Mehta, S., et al. (2011), ‘Mortality among cocaine users: a systematic review of cohort studies’, Drug and Alcohol Dependence 113 (2–3), pp. 88–95.
- de la Fuente, L., Molist, G., Espelt, A., Barrio, G., Guitart, A., Bravo, M.J., et al. (2013), ‘Mortality risk factors and excess mortality in a cohort of cocaine users admitted to drug treatment in Spain’, Journal of Substance Abuse Treatment 46(2), pp. 219–26.
Video: cocaine related emergencies
Facts and figures
2.2 million
2.2 million young adults (aged 15–34), or an average of 1.7%, used cocaine last year. Relatively high levels of cocaine use among young adults (between 2.4% and 3.6%) were reported in Denmark, Ireland, Spain and the United Kingdom.
22 years is the mean age at first use of cocaine, for the cocaine clients entering treatment in Europe. Their mean age at entering treatment is 33 years and 85% are male.
22
three
two- to three-fold: the increase in the number of cocaine-related episodes reported since the end of the 1990s in some countries.
2007 to 2008
2007–08 were the peak years for reports of cocaine-related emergencies in Spain and the United Kingdom.
27%
27% of the regular cocaine users (aged 18–20) in a recent Spanish study, who were not regular heroin users, had experienced acute cocaine toxicity symptoms during the last year. One-third of these (35%) presented symptoms of psychosis (hallucinations or delirium) and more than 50% reported chest pain (Santos, 2012).
A vignette of typical victims of a cocaine-related emergency in northern Italy

This vignette of typical victims of a cocaine-related emergency in northern Italy (1) is based on Pavarin et al., 2011 .
Hospitals based in the Emilia-Romagna region of northern Italy typically see two types of cocaine user presenting at emergency departments. The more common could be described as ‘non-dependent cocaine users’, probably using the drug recreationally. These represent around 80% of all cocaine-related cases. The remaining 20% of cases may be described as involving ‘dependent’ concurrent users of cocaine and opiates.
A typical ‘non-dependent’ emergency department visitor would be a man in his early thirties. He would have presented at the emergency department during the weekend, either at night or in the early hours of the morning (between 5 p.m. and 8 a.m.). He would have used cocaine more than 12 hours before presenting at the hospital, and may have used other substances alongside cocaine, particularly alcohol and cannabis. He would be suffering from one or more psychiatric symptom, in particular anxiety, agitation and paranoia. In addition, he may be feeling unwell and weak, with other symptoms including palpitations, chest pain and dyspnoea (difficulty in breathing), headache, vomiting and abdominal pain. He may also have presented with injuries (mainly unintentional) caused by violent behaviour or a road traffic accident.
By contrast, a typical ´dependent´ cocaine user visiting the emergency department would be a slightly older man, in his mid-thirties. He would have presented either at night or in the early hours of the morning, and not necessarily at the weekend. He would be using opiates regularly, together with cocaine and other drugs. With regard to symptoms, he is likely to be anxious, agitated and confused and might have hallucinations. He might present with palpitations, chest pain, vomiting and abdominal pain. Dyspnoea would be slightly more frequent than among non-dependent cocaine users and might be linked with smoking crack cocaine. He is more likely than a ´non-dependent´ user to present with complications of HIV or hepatitis C virus infection, which is linked with his long-term drug injection behaviour.
- Emergency health consequences of cocaine use in Europe. A review of the monitoring of drug-related acute emergencies in 30 European countries
- Cocaine–related deaths in special and general mortality registries
- Driving Under the Influence of Drugs, Alcohol and Medicines in Europe — findings from the DRUID project
- Cocaine: a European Union perspective in the global context
Find out more
Further reading
- Emergency health consequences of cocaine use in Europe. A review of the monitoring of drug-related acute emergencies in 30 European countries
- Cocaine–related deaths in special and general mortality registries
- Driving Under the Influence of Drugs, Alcohol and Medicines in Europe — findings from the DRUID project
- Cocaine: a European Union perspective in the global context