Spotlight on… Health and social responses to drug problems during the Covid-19 pandemic

What is the issue?
On 11 March 2020, the World Health Organization declared COVID-19 a pandemic. Since then, the virus has claimed millions of lives and has transformed nearly every aspect of individual and collective reality. As with all areas of life, drug consumption, related harms and drug markets have been impacted, as have the services established to respond to drug-related problems.
To respond to information needs during the ongoing public health emergency the EMCDDA has worked with other EU agencies and national data providers to create resources for the rapid identification and sharing of information relevant to its stakeholder groups. While the lack of comprehensive data means that all conclusions must be made with caution and be regarded as preliminary, it is useful to reflect on this first glimpse into new developments emerging both during and in response to the pandemic, and which could have important implications for the future.
What is happening in Europe?
Drug markets
Reports from national law enforcement experts indicate that the drug market has been remarkably resilient to disruption caused by the pandemic:
- Discovery of synthetic drug production sites and levels of cannabis cultivation in European countries appeared relatively stable.
- At wholesale level some changes in routes and methods are reported, with more reliance on smuggling via intermodal containers and commercial supply chains.
- At retail market level, following disruption in early lockdowns, drug sellers and buyers adapted by increasing their use of encrypted messaging services, social media apps, online sources and mail and home delivery services.
Drug use
With some exceptions, overall levels of availability and use for many illicit substances were relatively stable when comparing 2019 with 2020, although reports varied by substance and country:
- In general terms, there appears to have been less consumer interest in drugs usually associated with recreational events, such as MDMA, and greater interest in drugs that are perceived by the user to be more suitable for home consumption or alone.
- Despite some reductions during the initial lockdown period, the easing of restrictions during the summer 2020 was associated with a rebound in stimulant drug use (including MDMA, cocaine and amphetamine) in some cities.
- Among the possible worrying developments associated with the pandemic is the observation that some countries may be seeing an increase in crack cocaine availability and use, and the increasing reports of cannabis adulterated with highly potent synthetic cannabinoids (with some outbreaks of acute harms and deaths associated with these substances).
- Growing concerns have also been noted about the misuse of benzodiazepines, either diverted from therapeutic use or benzodiazepines not licenced for medical use in Europe appearing on the illicit drug market.
How is Europe responding?
Overall, drug services reported rapid adaptation, innovation and increased service flexibility:
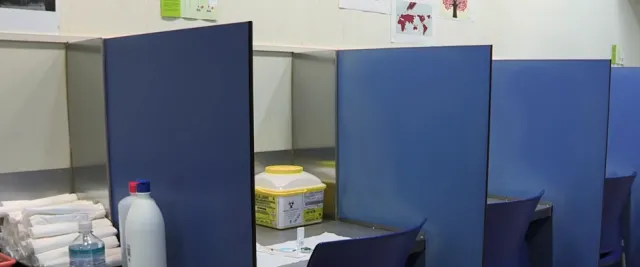
- Drug services across Europe, including low-threshold services, drug consumption rooms, and residential and outpatient treatment services, returned to operation in most countries from June 2020 onwards, although with strict COVID-19 measures in place and reduced capacity.
- Harm-reduction services have also been swift to adapt, playing a key role in providing frontline support during the crisis. This included: increasing outreach work and needle- and syringe-exchange activities; providing shelter management for homeless and marginalised groups; maintaining drug consumption room services (in situ or mobile) and moving some interventions online (e.g. drug checking).
- The provision of OST continued to remain high, and adaptations made during the first months of the pandemic — greater use of electronic prescriptions, greater quantities for take-home use, online supervision and low-threshold access — were maintained after the first confinement period.
- In six countries that reported monthly data for 2020, the numbers entering treatment fell sharply between February and March, and remained at low levels for the rest of the year. A greater use of telemedicine may have contributed to the reduction in reported treatment demand but also allowed services to continue to meet their clients’ needs during the pandemic.
- While many professionals report positive experiences of rapid adaptation and moving services online, some concerns are raised about reduced accessibility of telemedicine for certain client groups and associated challenges for treatment retention.
- Repeated school closures and online schooling proved challenging for implementing prevention and health promoting programmes during the pandemic.
- In most European countries, the provision of drug services in prisons remained reduced throughout 2020, although efforts were made to maintain the provision of opioid substitution treatment as well as testing and treatment for infectious diseases.
Implications for the future
- In the future there will be a need to pay close attention to the psychological and socioeconomic impacts of the pandemic, as well as longer term changes in patterns of illicit drug use and risk behaviours among the wider population.
- Drug problems are often found in marginalised groups such as the homeless, and those with drug problems may often rely on the informal economy. It is likely that these groups have been financially disadvantaged by social distancing measures and may be particularly vulnerable to any future economic difficulties resulting from the current crisis.
- The shift to the greater use of online platforms for the clinical management of drug problems will undoubtedly persist beyond the pandemic. However, the legal background of online/ phone treatment provision remains unclear in most countries, raising issues around client privacy and confidentiality.
- Ensuring the ongoing provision of drug treatment services during pandemics, including opioid substitution medications and other essential medicines to clients, will be a paramount consideration. Contingency plans will be needed for potential medication and equipment shortages and to guarantee the continuity of core health services to drug users. In this context, it is vital to ensure that services are properly resourced, staff protection measures are in place and service planning is prioritised.
See Impact of COVID-19 on drug markets, use, harms and drug services in the community and prisons, EMCDDA 2021.