Older people and drugs: health and social responses
Introduction
This miniguide is one of a larger set, which together comprise Health and social responses to drug problems: a European guide. It provides an overview of the most important aspects to consider when planning or delivering health and social responses for older people using drugs, and reviews the availability and effectiveness of the responses. It also considers implications for policy and practice.
Last update: 24 July 2023

Contents:
Overview
Key issues
Europe overall has an ageing population and people over the age of 40 make up an increasing share of those with an opioid problem. This is reflected in the increasing age of those in drug treatment and those dying from opioid overdoses. The problematic use of other drugs, for example benzodiazepines, is increasingly also causing concern.
In older people who use opioids, the physical ageing process may be accelerated by the cumulative effects of polydrug use and poor health over many years. These individuals may also be more susceptible to infection, overdose and suicide.
In addition, their social networks may be reduced because of premature death and stigma, which can further increase social exclusion and isolation from families. Stigma may also act as a barrier to help-seeking
Responses
There are currently few interventions targeting the specific needs of older people who use drugs and the evidence base for these interventions needs to be developed. Key responses may include:
- drug treatment services tailored to the needs of older people that provide multidisciplinary care to address their medical and psychological needs as well as their social isolation;
- improved access to, and uptake of, hepatitis C antiviral therapies;
- appropriate physical healthcare, including dental health services;
- awareness-raising and training of health and social care staff dealing with elderly people on how to respond to the needs of older people with drug problems, to ensure appropriate care and avoid stigmatisation;
- specialised nursing homes for the long-term residential care of ageing people who use drugs;
- advocacy support to increase self-esteem, acceptance and positive feelings about the future, including peer-led approaches;
- provision of safe and suitable housing.
European picture
Treatment and care for older people with drug problems is limited in Europe because most services were established to meet the needs of a younger cohort. Specialised nursing homes for older people with drug problems who are not able to care for themselves exist in only a small number of countries in Europe.
The planning of services to meet the future health and social care needs of the growing number of older people who use drugs in Europe will require age-specialised care services; an integrated, multidisciplinary approach with interagency partnerships; and referral between specialised and mainstream health and social services.
Key issues related to older people and drug use
Older people with drug problems are here considered to be those aged 40 or over whose long-term drug use is causing them harm or is placing them at a high risk of such harm. However, some of the issues discussed are relevant to older cohorts of people with drug problems who are at or beyond retirement age. They may well encounter negative life outcomes due to their drug use and have characteristics and trajectories distinct from those of their younger counterparts.
Older people with long-term patterns of opioid use make up an increasing proportion of people who use opioids in Europe. Over the past two decades, the average age of clients entering treatment for opioid-related problems has increased from the early thirties to the late thirties, while the average age of people dying from a drug-related death (mainly related to opioids) has also increased. The number of older people with drug problems in need of health and social care will continue to increase in the coming years, and this is particularly the case in the Western European countries that saw the first heroin epidemics in the 1980s and 1990s. In this context, there is an increasing need to develop responsive policies, treatment and services to support the needs of this population in Europe.
A wide range of health conditions can reduce the quality of life of those who have long histories of drug use. A large proportion of older people with problematic drug use in Europe initiated heroin use during the 1980s and 1990s. Many of those with long injecting careers have contracted HIV and hepatitis C virus (HCV) infections. Improved treatments are helping people with these infections to live longer, but their long history of problematic drug use may also have accelerated their physical ageing. Typically, this group have higher rates of somatic and mental health problems than their non-drug-using peers and younger people who use drugs. Earlier onsets of degenerative disorders, circulatory and respiratory problems, diabetes, hepatitis and liver cirrhosis are also possible. These individuals can also be more at risk of drug-related infections, overdose and suicide. In addition, mental health problems may be a serious concern.
Many older people who use opioids receive, or have received, methadone or buprenorphine treatment. However, little is currently known about the interaction and efficacy of opioid medication and treatments for people with physical disorders and impaired liver function. Providing suitable pain relief to older people who use opioids can be difficult for generic healthcare providers because these patients may have increased tolerance to opioid analgesics, and in the absence of guidance on effective pain management for this group, there is a risk that health services may undermedicate them. It is important that healthcare providers are aware that a number of the drugs that may be prescribed to people with problem opioid use, often alongside opioid substitution treatment, can increase the risk of overdose due to their depressant effects on the central nervous system. These include gabapentinoid drugs, prescribed for neuropathic pain, and benzodiazepines.
Rates of blood-borne viral infections are generally high among older people who have had long opioid-injecting careers, and older people who use opioids who contracted HCV early in their lives are at a greater risk of developing liver disease and cancer if they are not treated.
A significant proportion of older people with drug problems live alone, are in need of housing and are unemployed and economically inactive. Lack of employment reduces social networks, skills and knowledge and entrenches marginalisation and isolation. Stigma and ageism (discrimination on the grounds of age) add to the social exclusion and isolation from families and friends that are common in this group. These individuals are vulnerable to depression and loneliness because their social networks shrink as other older people who use drugs die or recover from addiction and move on. The stigma they may experience from continuing to use drugs as they advance into older age can prevent help-seeking, engaging with recovery communities and seeking healthcare.
Although the focus of the miniguide is mainly on older people with problems associated with opioid use, often alongside other drugs and alcohol, there are also groups of older people who use other drugs, for example cannabis and medicines such as benzodiazepines, in a problematic way. Older adults may have increased sensitivity to benzodiazepines and related medicines and a decreased ability to metabolise some longer-acting agents, such as diazepam. These drugs also increase the risk of cognitive impairment, delirium, falls and accidents. While in the past less attention has been paid to the problems of older people using these other drugs, some of the responses discussed here for people who use opioids may also be relevant to these groups, and some specific services, as well as greater involvement of primary care, may be needed. New guidelines on the prevention, assessment and treatment of problems are starting to be developed for service provision specific to these groups.
Responses to drug-related problems among older people
The scaling-up of harm reduction services in many European countries has kept people with heroin use problems alive into their later years. In general, older people who use opioids are treated within mainstream drug services. There are some interventions that target their specific needs, but a strong evidence base for these interventions is yet to be developed. Key responses for this population may include:
- drug treatment services tailored to the needs of older people, providing multidisciplinary care to address their medical and psychological needs as well as their social isolation;
- appropriate physical healthcare, including dental health services;
- improved access to, and uptake of, hepatitis C antiviral therapies;
- specialised nursing homes for the long-term residential care of ageing people who use drugs;
- provision of safe and adapted housing;
- awareness-raising and training of health and social care staff working with elderly people on how to respond to the needs of clients with drug problems, to ensure appropriate care and avoid stigmatisation;
- interventions to address social isolation and tackle stigma.
Integrated care tailored to the needs of older people
The planning of services to meet the future health and social care needs of the growing number of older people who use drugs in Europe may require age-specialised care services; an integrated, multidisciplinary approach with interagency partnerships; and referral between specialised and mainstream health and social services. Such a joined-up treatment approach for older people with drug problems, with interagency partnerships and established referral pathways between specialised and mainstream health and social services, will be particularly important. Training may need to be provided to staff in mainstream services for the successful implementation of these models of care.
There is currently a lack of tailored screening tools and treatment outcome measures for older people with substance use problems. The practical steps involved in supporting stabilisation or achieving recovery may differ for older and younger people who use drugs; for example, services might consider supervised methadone consumption in the homes of older people who use opioids or allow more take-home doses. Involving older people who use drugs in the development of these services will be important in ensuring that the services meet their needs.
In addition, drug treatment services may increasingly be required to respond to the needs of older people experiencing problems associated with use of other substances, such as benzodiazepines and possibly cannabis, who may also require tailored services. This may require having age-specific groups in services, hosting social activities and events, and providing regular peer and volunteer support to address social isolation.
Appropriate physical healthcare, including dental health services
Physically accessing services can be challenging for older people with opioid problems, who may require assistance with transport. Home visits may be provided to those with mobility problems or who live in rural areas, as well as satellite services operating out of community centres for older people and expanded outreach work.
Multidisciplinary and innovative approaches are key to addressing other medical (including dental), psychological and social needs of older people with drug problems.
Improved access to, and uptake of, hepatitis C antiviral therapies
Improved access to, and uptake of, such therapies in this population is likely to play a key role. In addition, their elevated risk of overdose death makes them an important target for take-home naloxone distribution and other overdose prevention strategies.
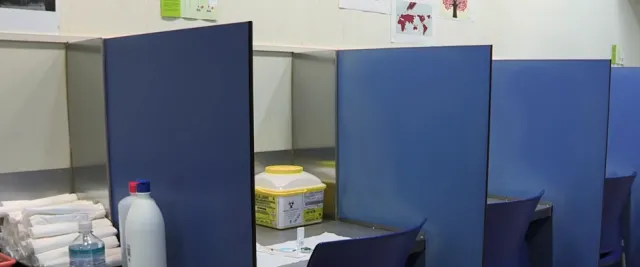
Specialised nursing homes for the long-term residential care of ageing people who use drugs
Some specialised nursing homes do exist for older people with drug problems who are not able to care for themselves. Alternatively, those with drug problems can be integrated into geriatric inpatient units and community old age settings. In general, these non-specialist settings are ill-equipped to offer the comprehensive assessment, treatment and care that older people with drug problems might need. Having a basic understanding of issues related to substance use and how it can impact the needs of elderly clients is increasingly required among staff working in this sector.
Provision of safe and adapted housing
More generally, safe and suitable housing is a prerequisite for dealing with social, health and physical challenges. The accommodation needs of older people who use drugs will often require particular attention for those choosing to move away from their drug-using networks. Those continuing to use drugs may require accommodation in which tenure is not threatened by drug use. Housing-first models, which provide accommodation before tackling an individual’s drug problem or providing other support, may be useful for older people who experience homelessness and use drugs (see Homelessness and drugs: health and social responses). Suitable housing for this group of the population may need to have universal access in order to accommodate eventual disabilities. In addition, employment and work programmes could provide some older people who use drugs with secure paid or voluntary work. Employers may require training to understand the health and social issues faced by this population.
Awareness-raising and training of health and social care staff
Training could also be provided to the geriatric care workforce to deal with the increasing numbers of these patients. Pain clinic staff and those providing end-of-life care may benefit from specialist training in managing pain in those who are opioid dependent, based around clear treatment protocols. There is currently a gap in the evidence base concerning effective practice in this area; nevertheless, a skilled workforce is important for improving the recognition of, and service provision for, older people with opioid problems.
Interventions to address social isolation and tackle stigma
Social isolation and loneliness in this group can be tackled by enhancing coping strategies, improving social networks and encouraging activities that enhance well-being. A pilot study in the United Kingdom showed that older people who use drugs could be recruited into a gym-based exercise scheme, but multiple social challenges reduced their ability to participate. Men’s Shed programmes in Australia, Canada, Ireland and the United Kingdom have encouraged older men to develop a sense of identity, self-esteem and value by learning new skills, developing social networks and engaging with communities.
To tackle the ageism and stigma experienced by many older people who use drugs, advocacy support can be provided by older peers within substance use services. Peer support can increase self-esteem, feelings of being accepted and understood, and positive feelings about the future. Those in a peer/volunteer role are also likely to benefit from this kind of engagement. Interventions engaging people back into society and helping them to develop or expand social networks can help to prevent loneliness and isolation among this group when implemented early in the treatment.
The evidence base for specialised responses to older opioid users is currently very limited. However, given the fact that in the longer-term, people aged over 40 who use opioids are likely to make up the majority of the drug treatment population in Europe, it is important that this issue is addressed and that effective interventions are developed to better inform policies and approaches. A limited number of guidelines for responding to this group exist: one initiative in Europe has been the development, by the European AIDS Clinical Society, of a set of guidelines in which there is an overview of interactions of HIV/AIDS treatment medications with other pharmacological treatments, including opioid agonist treatment (1). The guidelines are reviewed every other year, are published in a number of European languages, and can support clinicians in providing treatment and care that is more suitable to the needs of this population.
European picture: availability of drug-related interventions for older people
The provision of dedicated treatment and care services for older people with drug problems is limited and patchy in Europe. Most services were established to meet the needs of a younger cohort of people who use drugs, and clients have typically remained in these mainstream services over the years.
Specialised nursing homes for older people with drug problems who are not able to care for themselves do exist, for example in Belgium, Denmark, Germany and the Netherlands, but remain rare. They can serve as models for long-term residential programmes that offer care and support to chronic, ageing people who use drugs. An example from Germany is Condrobs, a service that offers low-threshold and acceptance-oriented support to older people using drugs. It provides counselling services, a residential care facility and a work project. Another example is the Geriatric Addiction Program, which was specifically developed to meet the needs of older adults in the United States who have substance use problems. It is a community-based programme providing in-home substance use intervention, assessment and linkage to services for older adults.
There are some limited examples of training being provided to help the workforce deal with the increasing numbers of these patients. BeTrAD (Better Treatment for Ageing Drug Users) is a project involving nine partner organisations in five EU countries, supported by the European Commission. The project provides adult trainers and organisations in the drug help system, in geriatric institutions and in local governments with the tools and models of good practice to create adult learning opportunities for the establishment and improvement of services for ageing people who use drugs. BeTrAD has developed a training curriculum for professionals in nursing care, addiction care and the medical system, alongside coordinators of self-help groups, reflecting a project focus on the inclusion of people who use drugs.
Implications for policy and practice
Basics
- Key issues for service providers include modifying or restructuring drug services and developing specialist services that address both health and social care needs of older people who use drugs.
- Clear communication channels and referral pathways need to be in place between drug services and mainstream health and social care services.
Opportunities
- Investment in workforce development for staff involved in generic elderly care, in order to improve their understanding of the needs of older people with drug problems, could improve the management of physical and mental health problems in this group.
- Developing protocols for managing pain in people who are opioid dependent for use in pain and palliative care clinics would assist the provision of high-quality care in these settings. Research is needed to provide evidence of good practice in this area.
Gaps
- Screening tools and outcome measures need to be developed that are appropriate for older people with long-standing substance misuse and associated health and social problems.
- There is a need to identify promising interventions and models of care to address the health and social problems experienced by the growing cohort of older people with opioid problems and to evaluate them to identify and share best practice.
- Responses will need to be developed to better meet the needs of older people who use substances other than heroin, including those using cannabis and stimulants.
Further resources
EMCDDA
- Responding to the needs of ageing drug users, 2017
- Ageing and addiction: challenges for treatment systems, 2015
Other sources
- European AIDS Clinical Society, Guidelines for the management of people living with HIV (PLWH) in Europe, 2022
- International Narcotics Control Board, A hidden epidemic: the use of drugs among older persons, 2020
- National Institute on Drug Abuse, Substance use in older adults: facts, 2020
- Scottish Drug Forum, Older people with drug problems in Scotland: addressing the needs of an ageing population, 2019
- Canadian Coalition for Seniors’ Mental Health, Guidelines on opiate use disorder among older adults, 2019
- Advisory Council on the Misuse of Drugs, Ageing cohort of drug users, 2017
- BeTrAD (Better Treatment for Ageing Drug Users), Toolbox, 2016
(1) The term ‘opioid agonist treatment’ is used here as the preferred language to cover a range of treatments that involve the prescription of opioid agonists to treat opioid dependence. The reader should be aware this term includes opioid substitution treatment (OST), a term that may still be used in some of our data collection tools and historical documents.
About this miniguide
This miniguide is one of a larger set, which together comprise Health and social responses to drug problems: a European guide. It provides an overview of the most important aspects to consider when planning or delivering health and social responses for older people using drugs, and reviews the availability and effectiveness of the responses. It also considers implications for policy and practice.
Recommended citation: European Monitoring Centre for Drugs and Drug Addiction (2023), Older people and drugs: health and social responses, https://www.emcdda.europa.eu/publications/mini-guides/older-people-and-….
Identifiers
HTML: TD-07-23-285-EN-Q
ISBN: 978-92-9497-864-6
DOI: 10.2810/684992