Workplaces and drugs: health and social responses
Introduction
This miniguide is one of a larger set, which together comprise Health and social responses to drug problems: a European guide. It provides an overview of what to consider when planning or delivering health and social responses to drug-related problems at the workplace, and reviews the available interventions and their effectiveness. It also considers implications for policy and practice.
Last update: March 2022.

Contents:
Overview
Key issues
A significant proportion of workers in Europe are likely to have problems associated with alcohol or drug use; for example, it is estimated that between 5 % and 20 % of the working population in Europe have serious problems related to their use of alcohol. In addition to the general public health and social implications, substance use problems are highly relevant in industries which involve safety issues or where individual performance failings can have a significant impact. This includes, but is not limited to, the construction, farming, transport, power, ICT and financial services sectors.
Alcohol and drug use are important issues in workplaces because:
- they can increase accidents and injuries, absenteeism and inappropriate behaviour;
- they can impose an economic burden on employers, governments and society;
- employers have a duty under health and safety laws to protect, as far as reasonable, the health, safety and welfare of employees and others affected by their activities;
- workplaces also provide opportunities for health education about alcohol and drugs and to identify individuals who have problems with alcohol and drug use or have family members with drug or alcohol problems.
The workplace also has a potential role in supporting the social reintegration of people with a history of drug problems.
Evidence and responses
There is no comprehensive overview of the extent and nature of different types of interventions in workplaces in Europe. Moreover, the evidence regarding effectiveness of different interventions is scarce. Responses implemented may include:
- company policies focusing on the consumption of alcohol and drugs in the workplace and support for employees with substance use problems;
- prevention through information, education and training programmes addressing alcohol and drugs issues, preferably as part of wider health promotion programmes;
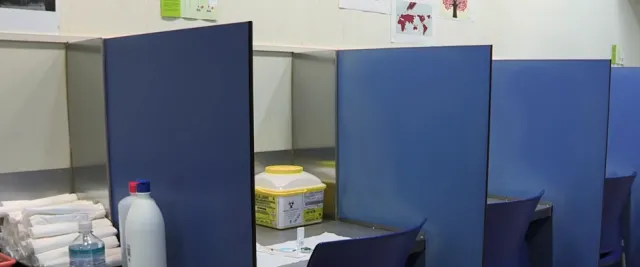
- formal screening and drug testing in safety-critical industries;
- interventions to identify employees experiencing substance-related problems and provide support for them, including the facilitation of referral to treatment and rehabilitation programmes;
- actions exploring organisational-level factors that may be contributing to drug-related problems among the workforce;
- providing employment opportunities for people with a history of drug problems.
European picture
Most European countries have some kind of general legislation or agreements to prohibit or regulate the consumption of alcohol and drugs in the workplace. However, the type of legislation in force and the nature of occupational safety and health legislation varies considerably depending on the national culture and the awareness of and priority given to the issue.
Looking to the future, the use of human enhancement drugs, such as modafinil for improving cognitive function, may become a growing issue in the workplace.
Key issues related to drug use and the workplace
Alcohol and drugs represent a serious problem for a substantial share of the working population. National estimates in Europe indicate that between 5 % and 20 % of workers are either dependent on alcohol or at risk of becoming so. While concerns continue to focus on the impact of alcohol, established illicit drugs and some prescription drugs, new challenges are emerging linked to perceived performance enhancers.
Alcohol and drug use can exacerbate potential problems in the workplace, such as accidents and injuries, absenteeism and inappropriate behaviour. Intoxication by alcohol or drugs can affect work performance by impairing decision-making and reaction times, reducing productivity and leading to the production of inferior goods and services, and errors and workplace accidents.
The reasons for using alcohol or drugs at work can be differentiated into work-related and social or personal categories. Work-related reasons include tough physical or uncomfortable working conditions (for example, a cold environment, long hours standing, extreme physical exertion), low satisfaction at work, irregular working hours and shift work. Other causes identified here include the perception of low social support from colleagues, little decision-making latitude and various factors related to stress at work. This could result in certain occupations being more likely to be linked to substance use. For example, long-distance lorry drivers, who need to stay awake and maintain concentration for long, monotonous periods of driving, may be at greater risk of using stimulant drugs. Doctors and other health professionals may be vulnerable to addiction problems due to having easy access to medicines, combined with long shifts and stress at work. Other groups of workers in high pressure, competitive or bullying work cultures, including city traders, academics and lawyers, may use a range of cognitive enhancers for a variety of reasons, such as to improve productivity or to overcome jetlag.
One area of emerging concern is the rapid growth in Europe and globally of short-term work arrangements and what is known as precarious work. Features of these working practices include lack of social/individual control over working conditions; the fragmentation of working times and spaces; overlapping or blurred boundaries between work and personal life or difficulty in achieving a balance between paid work and other aspects of life; conditions of competition, shortage of work and threats to one’s livelihood; and a high level of monitoring of employees. All of these factors may increase the likelihood of using substances in order to manage competing pressures and stresses.
Non-job-related reasons include social factors, such as a ‘high’ social tolerance to alcohol and drug consumption (the normalisation of substance use), cultural patterns that may make workers more likely to consume drugs, and employees having greater access to these substances (in the alcohol and entertainment industries, for example).
A number of ethical and often legal obligations are relevant to responding to workplace substance misuse problems. Organisational factors and working practices, as potential drivers of substance use, are relevant here. Medical professionals brought into a workplace to help employees or advise management have to clarify their role and respect patient confidentiality. It is generally accepted that managers and supervisors should be trained to recognise the signs of problematic alcohol or illicit drug use among their workforce. They also need to know how to respond if they suspect an employee has substance use problem or if they are approached by an employee who discloses that they have a problem. In addition, it is important to recognise that managers and supervisors may themselves have problems with alcohol and illicit drug use.
In supporting people with a past or current alcohol or drug problem back into work, health professionals play an important role. They can be very influential in addressing employers’ concerns about the risks involved and challenging stigma and negative stereotypes, as well as supporting managers in refraining from the application of arbitrary abstinence periods, except where they are legally mandated, such as for driving.
The use of human enhancement drugs in the workplace is an emerging issue. Human enhancement drugs are substances that have the perceived potential to improve human traits, appearance, mood or performance. There are several types of such substances, for example performance- and image-enhancing drugs (PIED) (see Spotlight on… Performance- and image-enhancing drugs), cognitive enhancers, sexual performance enhancers, and mood and behaviour enhancers. Cognitive enhancers, also known as ‘smart’ drugs, raise particular concerns in the workplace. These include medicines, such as Ritalin (methylphenidate), Provigil (modafinil) and Adderall (amphetamine salts), which may be used by individuals without prescriptions or medical supervision and taken in different doses than their recommended medical use, because they are believed to improve concentration and cognitive performance, although the evidence for this is limited.
More recently, media attention has highlighted the practice of ‘micro-dosing’ of hallucinogens such as LSD (lysergic acid diethylamide) to increase creativity, which is suggested to occur among groups of workers such as software developers. This is one example of the possible use of a wide range of other substances, drugs, supplements and nutritional products that are believed to improve aspects of mental function, known collectively as ‘nootropics’.
The expansion in the range of substances that may be used and the fact that some of these substances may be used legitimately – prescribed for medical conditions or sold legally in the case of alcohol and some novel psychoactive substances – complicates responses. Sources of supply have also diversified, with internet pharmacies, the darknet and social media in particular providing easier access to human enhancement drugs and other substances.
Evidence and responses to drug-related issues and the workplace
Action to address drug problems in the workplace initially aimed to improve safety at work, but has increasingly focused more on promoting the health and well-being of the workforce, which can also have benefits for the wider community. Workplaces provide opportunities for the provision of health education about alcohol and drugs. They also offer the possibility of identifying individuals who have a problem with alcohol or illicit drug use. Medical professionals who support workplaces are well placed to offer health advice to workers. They can also train managers and supervisors to recognise and deal with alcohol and illicit drug use in the workplace.
The International Labour Organization has produced a code of practice on the management of alcohol- and drug-related issues in the workplace. It places emphasis on prevention and takes a health-focused approach, as opposed to a disciplinary one. At the national level, approaches to drug-related problems in the workplace will be influenced by the administrative, legislative and cultural context in each country. Regulations, legislation and policies in the domains of employment law and health and safety may also be relevant to drug issues in the workplace. In addition, to support their policies, countries may produce their own guidance for employers.
The following responses may be used to address drug use and problems in the workplace. However, the way in which responses are provided and the main areas of focus will depend on both the sector and the type of work undertaken within the organisation, as well as its size. Large companies will have sizeable human resources departments and are likely to have access to specialists to deal with drug and alcohol issues. In small and medium-sized enterprises, it is usually the owner, managing director or site manager who takes care of health and safety issues.
- Workplace policies. All organisations can benefit from having a drugs policy alongside more general health and disciplinary protocols. A formal workplace drugs policy provides an opportunity to set an example and promote the provision of appropriate support and assistance to the workforce. The main focus should be on preventive interventions, and some policies place restrictions on the consumption of alcohol and drugs in the workplace, thereby establishing norms and limiting availability. There are different models of policy development, but involving employees in their creation in some form is generally considered good practice.
- Prevention through information, education and training programmes. Incorporating alcohol and drugs issues into wider health promotion programmes may make such programmes more attractive to employees. The communication of information about human enhancement drugs will need to raise awareness of the risks and dangers of these substances, without increasing their potential attractiveness.
- Formal screening for drug problems. This will generally occur in three situations: (1) pre-employment testing of job applicants; (2) incident-driven or for-cause testing of employees (e.g. post-accident, checking fitness for duty); and (3) in-employment testing without a specific cause, with subjects often selected at random from the pool of people in targeted safety-sensitive or safety-critical positions. The evidence for the effectiveness of testing in reducing accidents and improving job performance, however, is very limited, and the few studies that have been carried out are of poor quality. There are technical, ethical and legal challenges to testing programmes, which are growing as the range of substances involved is increasing and the lines between legal and illegal substance use become increasingly blurred.
- Identification of problems at the individual level. In workplaces without formal drug-testing requirements, the identification of drug problems will often arise either through self-disclosure by the individual concerned or as a result of discovery by the employer, either informally through discussions around performance issues or as a result of formal assessments. On identification of an issue, workplaces may offer a range of supportive interventions, including counselling and referral to specialist care. The aim here may be to provide options that offer help and support, and forestall disciplinary procedures or the dismissal of employees with substance use problems, usually contingent upon their ability to constructively address any issues that negatively affect job performance.
- Identification of problems at the organisational level. In collaboration with employees, it can be good practice for employers to work on identifying and addressing elements at the organisational level that may be contributing to drug-related problems. In addition, reviewing socialisation cultures in the organisation – after-work drinks, company staff events, events with clients, etc. – can inform changes in certain social practices that may not only protect employees seeking to curtail their consumption, but also provide a wider health benefit to other staff.
- Interventions to directly respond to substance-related problems. These interventions include counselling, referral to and funding of treatment and rehabilitation programmes. The type and level of support provided will depend on a range of factors, including the size of the organisation. Actions that should be considered as a minimum include identifying specialist services in the area and providing information on these or referral if appropriate; identifying community support agencies and self-help groups that may be helpful to the individual concerned; suggesting the individual seeks support from his or her personal physician.
The workplace also has a potential role in supporting the social reintegration of people with a history of problematic substance use. The stigma associated in particular with problematic drug use can pose a major barrier to employment, which is a cornerstone of reintegration. However, some employers have worked with local drug services to develop programmes, such as supported employment schemes, that facilitate the employment of people with a history of problematic drug use and report that these produce benefits for the organisation as well as the individual concerned.
European picture: availability of interventions responding to drug-related issues and the workplace
A European-level mapping of the practices and interventions relating to substance-related issues in the workplace has not been carried out in Europe. A report produced by European Foundation for the Improvement of Living and Working Conditions (Eurofound) in 2021 indicated that most European countries have some kind of general legislation or agreements in place that are intended to prohibit or regulate the consumption of alcohol and drugs in the workplace. However, the types of legislation in force and the nature of the limitations established under occupational health and safety regulations vary considerably depending on the national culture and the awareness of and priority given to the issue. For example, in some countries, there may be a specific regulation concerning alcohol, whereas in others it is left to the employer’s discretion. In addition, rules may be agreed between employers and employees in labour agreements and hence not appear in the corresponding national legal framework.
The Sundsvall model of policy development, developed in Sweden, became known as Workplace Against Drugs, and its reach extended beyond the workplace and into the community. It involved all workplaces in the region and comprised a number of activities designed to develop awareness of problem use in the workplace and the community, as well as training programmes for supervisors to facilitate the identification of problem drug use in both arenas. It also created help and support networks based around referral structures involving local services.
The evidence of effectiveness for the different programmes and interventions that are in use in Europe is also limited, and what little exists primarily comes from the United States. A comprehensive assessment of most current provision is therefore not possible.
However, there are data sources available that can provide some information, with both the European Agency for Safety and Health at Work (EU-OSHA) and Eurofound involved in the management of alcohol- and drug-related issues in the workplace. A common theme here is the importance of having a preventive approach that views drug problems from a health perspective rather than as a disciplinary issue. EU-OSHA, for example, conducts the European Survey of Enterprises on New and Emerging Risks (ESENER), which focuses on a number of issues: general safety and health risks in the workplace; psychosocial hazards, such as stress, bullying and harassment; drivers of and barriers to occupational safety and health management; and worker participation in health and safety practices. The survey was carried out in 2009, 2014 and 2019, and the data are available online. It found, for instance, that about a third of respondents across Europe work in companies where measures are taken for health promotion among employees, including raising awareness on the dangers of addiction to smoking, alcohol or drugs.
The European Network for Workplace Health Promotion (ENWHP) provides a platform for all stakeholders interested in the improvement of workers’ health and well-being. It seeks to encourage the development of workplace health promotion in Europe through influencing policy creation, establishing education and training programmes, providing accreditation and promoting research.
In Europe, responses have tended to focus on promoting workplace health and well-being; however, providing an overview of health and drug-related responses in the workplace is difficult. The approaches adopted may depend on local practice as well as cultural expectations and the size of the companies. Some organisations may provide training to all managers and supervisors on how to manage employees who may be using drugs, have substance misuse problems or are intoxicated at work, according to company policy and procedures. Others, particularly smaller companies, may employ external consultants to provide support for policy development, training and awareness raising. In Germany, for instance, the prevention programme ‘Top on Job’ targets young workers before addiction problems occur and uses a peer-education approach.
Some countries have established interventions to address substance use problems that have been identified among employees. In Belgium, for instance, a system of referral was established from the workplace to the family physician, who, when necessary, can refer the employee on to a specialist drug treatment service. The important point here is to facilitate links and referral options between drug services, workplaces and employees needing support.
Formal drug screening and testing in Europe is generally conducted only where necessary to promote workplace safety, for example in the transportation sector, the oil and nuclear industries, and in the armed services. Yet, there is little evidence on the effectiveness of drug testing in the workplace in terms of reducing work accidents and improving performance. The European Workplace Drug Testing Society (EWDTS) brings together users and providers of drug-testing services, facilitating a discussion forum for the exchange of ideas and information. It has also developed guidelines for the testing of oral fluid, urine and hair.
Looking to the future, the use of drugs for enhancement purposes may become a growing issue in the workplace. This includes the use of a wider range of drugs than has been seen previously, and it will be important to monitor the use of these substances in the future, particularly cognitive enhancers. Changes in working patterns, including increased teleworking during the COVID-19 pandemic and the growth of short-term working arrangements and precarious employment, often result in the loss of the traditional employer-employee relationship. People working under these conditions may be at high risk of drug and alcohol use to cope with the stress and strains of such work patterns, especially since they may have no fixed workplace or employer to take responsibility for supporting them and preventing problems from escalating. New preventive models for addressing their needs will need to be developed.
Implications for policy and practice
Basics
- It is recommended that employers have an alcohol- and drug-use policy as a component of their health and welfare policies rather than as a disciplinary matter.
- The key principles for the management of drug-related issues in the workplace identified by the UN International Labour Organization, and highlighted above, should also be promoted.
Opportunities
- Gaining employment is an important component of social reintegration. Therefore, it is important that people with a past or current alcohol or drug problem are supported back into work. Working with employers to overcome barriers to employing people with a history of drug problems offers benefits to the organisation, to those trying to overcome their drug problems and to society as a whole.
- Workplaces provide an opportunity to provide health education about alcohol and drugs and to identify and provide support for individuals with substance use problems.
Gaps
- There is a need for an overview or mapping of existing data sources, as well as current responses and interventions addressing drugs in the workplace, together with an evaluation of existing interventions in Europe.
- Research is needed into the extent and nature of the use of human enhancement drugs in the workplace and on the effects of their use.
- Where there might be no workplace as such or no employer-employee relationship, new preventive models for addressing the needs of workers will need to be developed.
Data and graphics

Data drawn from the Third European Survey on Enterprises on New and Emerging Risks, ESENER 2019, coordinated by EU-OSHA. A total of 45 420 establishments were surveyed on how health and safety risks are managed at their workplace, with a particular focus on psychosocial risks, i.e. work-related stress, violence and harassment.
Further resources
EMCDDA
- Social reintegration and employment: evidence and interventions for drug users in treatment. EMCDDA Insights, 2013.
Other sources
- Pompidou Group. Prevention of drug use in the workplace.
- European Agency for Safety and Health at Work. Managing performance-enhancing drugs in the workplace: An occupational safety and health perspective, Discussion paper, 2018.
- European Agency for Safety and Health at Work. A review on the future of work: performance-enhancing drugs, Discussion paper, 2015.
- European Agency for Safety and Health at Work. European survey of enterprises on new and emerging risks, 2014.
- European Foundation for the Improvement of Living and Working Conditions. Use of alcohol and drugs at the workplace, 2012.
- Shahandeh, B. and Caborn, J. Ethical issues in workplace drug testing in Europe. International Labour Office, Geneva, 2003.
- International Labour Office. Management of alcohol- and drug-related issues in the workplace. An ILO code of practice. ILO, Geneva, 1996.
About this miniguide
This miniguide provides an overview of what to consider when planning or delivering health and social responses to drug-related problems at the workplace, and reviews the available interventions and their effectiveness. It also considers implications for policy and practice. This miniguide is one of a larger set, which together comprise Health and Social Responses to Drug Problems: A European guide.
Recommended citation: European Monitoring Centre for Drugs and Drug Addiction (2022), Workplaces and drugs: health and social responses, https://www.emcdda.europa.eu/publications/mini-guides/workplaces-and-dr….
Identifiers
HTML: TD-09-22-044-EN-Q
ISBN: 978-92-9497-699-4
DOI: 10.2810/416043