Statistical Bulletin 2017 — overdose deaths
Archived content
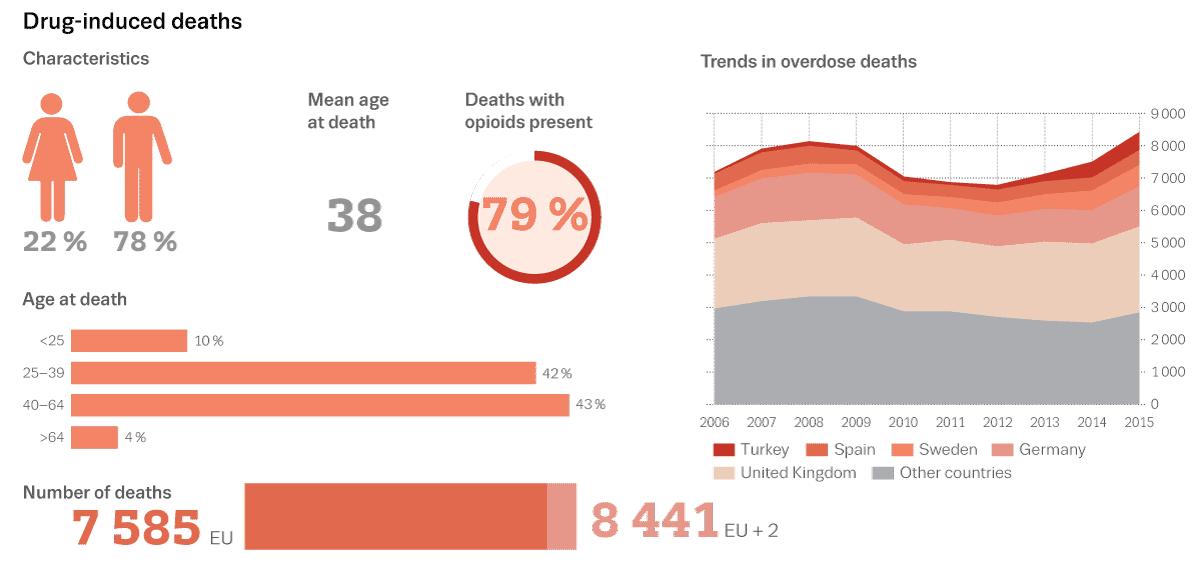
Drug-related mortality is a complex phenomenon, which accounts for a considerable percentage of deaths among young people in many European countries. The EMCDDA, in collaboration with national experts, has defined an epidemiological indicator with two components at present: deaths directly caused by illegal drugs (drug-induced deaths) and mortality rates among problem drug users. These two components can fulfil several public health objectives, notably as an indicator of the overall health impact of drug use and the components of this impact, identify particularly risky patterns of use, and potentially identify new risks.
Data tables
Use the menu below to find data sets of interest.
Graphics
Click on a graphic from the thumbnails below
Drug-related deaths and mortality — an overview of the methods and definitions used
The EMCDDA drug-related deaths (DRD) indicator focuses on deaths directly caused by illegal drugs (drug-induced deaths) and mortality among drug users across the European Union (EU) Member States, Norway and Turkey. The EMCDDA monitors national statistics on drug-induced deaths and reports the results in the Data and statistics section (Statistical Bulletin) of the European Drug Report (EDR).
The EMCDDA encourages countries to both harmonise their data collection and reporting (1). Nevertheless, differences in the availability of autopsies and in coding practices between countries will influence the interpretation and comparability of the results.
Users of the data should consider carefully the methods and definitions described below and the notes associated with the data in the Statistical Bulletin. The underlying protocol and guidance to data providers provide further information necessary when interpreting the data. The individual country National reports are a source of contextual and methodological information and the basis of much of the information here. All of the above are available on the EMCDDA website (see ‘Key links’ below).
The number of drug-induced deaths provides one perspective on the drug situation and should be considered within the broader range of information available. Cross-referencing between data-sets provides both additional insights and a check of validity. The DRD indicator also considers mortality amongst drug users derived from cohort studies. EMCDDA monitoring of problem drug use and treatment (treatment demand indicator, opioid substitution treatment) provides perspectives and information on the more intensive forms of drug use.
Purpose and aims
The general purpose of the indicator is to improve understanding of the health impact of different forms of drug use and its correlates and determinants, with the aim of informing the development and evaluation of policies and interventions designed to reduce health problems, in particular mortality, related to drug use.
Data on the number, characteristics (age, gender, intention) and circumstances of people dying as a direct result of drug-taking can fulfil several complementary purposes, especially when presented and interpreted alongside other drug indicators.
The particular purposes of this data include:
- to identify risky patterns of use (e.g. injection or polydrug use) and risk among the most vulnerable groups of problem drug users;
- to identify new risks, for example new substances, a combination of substances including medicines or contaminated or adulterated batches of drugs — this information can contribute to the risk assessment of new psychoactive substances;
- to help to monitor trends in the prevalence of specific drug problems with an elevated risk, such as injecting heroin use.
Definitions
The EMCDDA definition of drug-induced deaths is simple and relatively restrictive. It is defined within the DRD protocol as 'people who die directly due to use of illegal substances’, although these often occur in combination with other substances such as alcohol or psychoactive medicines. The deaths generally occur shortly after the consumption of the substance and are commonly referred to as overdoses or poisonings.
The EMCDDA standard protocol transforms this definition into operative criteria for extracting the deaths to be reported from both general mortality registers (GMR) and special registers (SR) (e.g. forensic, coroners’ registers). In GMR these operative criteria consist of a list of codes from the WHO International Classification of Diseases (ICD) 10th Edition (see ‘Key links’ below). Doctors, coroners and professional coders use them to code the cause(s) of death, based on the death certificates. The operative criteria for the SR consist of the classes of death that determine which cases should be reported (only overdoses, out of all possible cases recorded in these registries).
The EMCDDA recommends that the information is extracted from both systems (GMR and SR) if they exist in a country, to assess consistency and cross-validation. This is implemented in many countries.
For further details and definitions see the DRD protocol (see ‘Key links’ below).
Methods
The EMCDDA monitoring standards for drug-related deaths (drug-induced deaths) require the total number of cases of death attributed directly to the use of illegal substances of abuse to be collected at the national level. In addition, for each reported case, information is collected on the gender and age-band of the victim and on the substances that caused the death. Information on the presence and associations of different drugs, medicines, alcohol and other substances is also provided, when available (mainly when extracted from the SR).
The extracted data is then sent to the EMCDDA by means of an online data collection system called Fonte.
For GMRs the list of ICD-10 codes to be reported to the EMCDDA is known as ‘Selection B’. They include cases where the underlying cause of death (the condition that initiated the process that lead to the death) are: (i) mental and behavioural disorders due to psychoactive substance use (harmful use, dependence and other mental and behavioural disorders (F codes) due to opioids, cannabinoids, cocaine, other stimulants, hallucinogens or multiple drug use; or (ii) poisonings (X and Y codes) that are accidental, intentional or of undetermined intent due to substances under the heading of narcotics (T40-0 to T40-9) or psychostimulants (T43.6).
For SRs the EMCDDA operative criteria are known as ‘Selection D’. Cases are selected when the death are due to poisoning by accident, suicide, homicide or undetermined intent by a set of illegal drugs of abuse.
At present, national mortality statistics are improving in most countries and their definitions are becoming more comparable, or with slight differences, to the common EMCDDA definitions.
Cases to be extracted from the mortality registries
In operative terms the cases are identified and selected as follows:
1. By extraction of the cases from GMRs according to the following criteria (Selection B):
- based on the WHO International Classification of Diseases, 9th edition (ICD-9);
- based on the WHO International Classification of Diseases, 10th edition (ICD-10).
Case are counted when their underlying cause of death is mental and behavioral disorders due to psychoactive substance use (see below) or poisoning (accidental, intentional or by undetermined intent):
- harmful use, dependence, and other mental and behavioural disorders due to: opioids (F11), cannabinoids (F12), cocaine (F14), other stimulants (F15), hallucinogens (F16), multiple drug use (F19);
- accidental poisoning (X41, X42), intentional poisoning (X61, X62), or poisoning by undetermined intent (Y11, Y12) by: opium (T40.0), heroin (T40.1), other opioids (T40.2), methadone (T40.3), other synthetic narcotics (T40.4), cocaine (T40.5), other and unspecified narcotics (T40.6), cannabis (T40.7), lysergide (T40.8), other and unspecified psychodysleptics (T40.9), psychostimulants (T43.6).
The T-codes are to be selected in combination with the respective X-codes and Y-codes.
| Underlying cause of death | Selected ICD-10 code(s) |
|---|---|
| Disorders | F11–F12, F14–F16, and F19 |
| Accidental poisoning | X42 (1), X41 (2) |
| Intentional poisoning | X62 (1), X61 (2) |
| Poisoning, undetermined intent | Y12 (1), Y11 (2) |
(1) In combination with T-codes: T40.0–40.9.
(2) In combination with T-code: T43.6.
Effect of the ICD-10 updates
Several ICD-10 updates for codification of deaths due to drug intoxications were adopted by the World Health Organization (WHO) in 2002 and 2003 by the Heads of WHO Collaborating Centres for International Classifications in Health Care and these entered into force in 2006. Some additional combination of codes should be included for countries that have already implemented these ICD-10 updates: X44, X64 and Y14 in combination with main injury codes (T-codes) T40.0–40.9 and T43.6.
Note that X44, X64 and Y14 alone, not in combination with T codes, or without the implementation of the updates, are not part of the DRD standard.
2. By extraction of the cases from SRs (forensic or police registries) (Selection D)
This method is applied in countries where the previous method cannot be implemented, but also whenever possible as a backup estimate and validation of the numbers derived from the GMRs. Cases are counted when the death is due to poisoning (by accident, suicide, homicide or of undetermined intent), and when the death is due to opiates, amphetamines, cocaine (or crack), cannabis, hallucinogens, solvents, or synthetic designer drugs such as amphetamine derivatives.
The specific groups of deaths to be selected are:
| Category of drug-related death | Selected groups |
|---|---|
| Poisoning by accident, suicide, homicide, or undetermined intent | Opiates only (excluding methadone only) |
| Methadone only | |
| Poly-substances (1) including opiates | |
| Poly-substances excluding opiates | |
| Unspecified/unknown (2) |
(1) 'Poly-substances' should include at least one of the above-mentioned seven substances or categories of substances.
(2) 'Unspecified/unknown' is used when the case is assumed to include at least one of the above-mentioned substances.
Limitations
The key factors in the quality of the data on drug-induced deaths are the availability and nature of post-mortem investigations and the full use of this information for death certification and coding. The comparability of the national figures depends on the harmonisation of coding practices at national levels.
Notable issues related to coding include the following:
- There are country differences in which codes are applied. In particular, in some countries T codes are never or rarely used, whereas in others they are more frequently used. Where T codes are not applied, the number of drug-induced deaths would be an underestimate.
- A few countries still include cases due to psychoactive medicines or non-overdose deaths, generally as a limited proportion of the total.
- The GMR will not identify the presence of new psychoactive substances as there are no specific codes in the ICD-10 to code these substances. Deaths involving these substances would be coded with more general codes such as ‘other stimulants’.
In addition, there are still differences between countries in procedures for recording cases, and in the frequency of post-mortem toxicological investigations. Information exchange between GMRs and SRs (forensic or police) is insufficient or lacking in some countries, which may compromise the completeness of the information.
The difference in the national practices of coding the causes of deaths implies that direct comparisons between countries in the numbers or rates of DRDs should be made with caution. However, the trends observed can give valuable insight if methods are maintained consistently within a country, especially when interpreted together with other drug indicators.
Available information on the codes used to classify drug-induced deaths has been compiled by country to aid interpretation of the data. Cross referencing with EMCDDA and other data collections is recommended.
Key links
For further information please refer to the following:
- DRD protocol
- DRD web page
- Country Drug Reports
- Data collection template: Most recent data | Time series | Cohort data
- WHO International Classification of Diseases, 10th edition.
Key publications
- EMCDDA (2011), Mortality related to drug use in Europe, EMCDDA, Lisbon.
- EMCDDA (2012), Cocaine-related deaths in special and general mortality registries, EMCDDA, Lisbon.
- EMCDDA (2012), Mortality cohort guidelines, EMCDDA, Lisbon.
- EMCDDA (2015), Mortality among drug users in Europe: new and old challenges for public health, EMCDDA, Lisbon.
- Preventing overdose deaths in Europe (Perspectives on Drugs), 2016
References to most recent work
- New technical reports are made available on the DRD activies page (under 'Studies')
- EMCDDA expert meeting on the epidemiological indicator: Drug-related deaths (DRD)
(1) The EMCDDA publishes a detailed protocol on how to collect DRD, holds annual meetings of both experts and data providers, provides direct assistance to data providers, and monitors and reviews the academic literature. Further information is available on the EMCDDA website.